What is Interstitial Lung Disease (ILD) / Pulmonary Fibrosis?
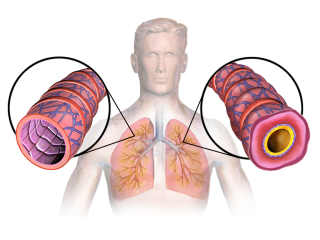
Interstitial lung disease may also be referred to as pulmonary fibrosis. This disease involves scarring and inflammation of the tissue around the lungs, known as the interstitium. The scarring seen in pulmonary fibrosis can make these normally pliable tissues around the lungs stiff and inflexible, which can ultimately cause problems with breathing. In addition, the scarring inhibits the natural flow of oxygen and carbon dioxide to and from the lungs, leading to a diminished amount of oxygen in the lungs and bloodstream (and also, ultimately, higher levels of carbon dioxide).Symptoms of ILD include:
- Coughing
- Shortness of breath
- Fatigue
- Weight loss
- Decreased tolerance during exercise or physical activity
- High blood pressure (specifically in the lungs)
- Sleep disorders
In many people, pulmonary fibrosis develops concurrently with another illness. For example, people with autoimmune diseases like rheumatoid arthritis, lupus, sarcoidosis, scleroderma, and others. Some genetic diseases may also predispose a person to developing ILD (examples include Gaucher disease and neurofibromatosis). Regular exposure to certain chemicals can also lead to a higher likelihood of developing interstitial lung disease.
Note that in cases where pulmonary fibrosis presents alongside an autoimmune disorder, because these two health problems are so intimately intertwined, it will be important to treat both at the same time in order to maximize success, ideally while using a healing protocol to approach the situation from a few different directions.
Treatments for Interstitial Lung Disease
Halotherapy for Interstitial Lung Disease
Halotherapy is a treatment done using salt (sodium chloride) as the primary medicine. In this treatment, patients will visit a manmade salt “cave” (though natural salt caves do exist, and patients can go to one of of these natural caves if there is one nearby to experience the same benefits). The salt cave is kept at a temperature of 68 degrees Fahrenheit and dehumidified, meanwhile a halogenerator grinds up natural salt into tiny particles, which are then released into the air for the recipient to breathe during their session. Most sessions last between 15-45 minutes, though some studies into the use of halotherapy for lung diseases recommend 60 minutes daily for 10-25 days in a row (with this being repeated up to 2 times a year for best results). Living by the ocean or right next to a body of saltwater may also offer some similar (though perhaps less significant) benefits for patients with lung problems.Halotherapy is very safe, and little to no adverse effects have been observed in patients of any age . Even young children and very elderly people can use halotherapy safely for health and healing without having to worry about side effects. Some people do note that they develop a headache during their halotherapy session, however I’m inclined to believe that this is probably a result of some kind of sinus clearing.
According to experts on this therapy, halotherapy works by absorbing allergens and toxins (such as bacteria, chemicals, or viruses) present in the respiratory system. This then allows the body to break up and purge excess mucus more effectively and can also reduce inflammation (toxins and allergens can cause inflammation of the respiratory system, and thus, when the salt absorbs them, they no longer pose a threat and the respiratory tissues don’t have to stay inflamed).
Nebulization/Inhalation of Molecular Hydrogen Water Daily
Molecular hydrogen may be administered at home or at a facility for the treatment of pulmonary fibrosis, as well as for the treatment of other lung diseases, including COPD, asthma, and emphysema in particular. Hydrogen gas is sometimes administered in place of oxygen therapy (discussed more below) in the same way as oxygen therapy by administering hydrogen gas directly into the airways through a cannula in the nostrils. However, molecular hydrogen may also be taken through nebulization or inhalation of molecular hydrogen water, which is generally one of the best ways for patients with lung problems to be able to self-administer this medicine at home or under the supervision of a healthcare professional.Molecular hydrogen may also be drunk in water, added to a bath or footbath, or administered intravenously at a clinic.
 Molecular hydrogen acts quickly to stop and even reverse the effects of oxidative stress in the body, and can also reduce inflammation and allergic reactions in the respiratory system. Since interstitial lung disease involves oxidation of the tissues surrounding the lungs (and subsequent scarring and stiffening of these tissues), use of molecular hydrogen administered by nebulization may be able to stop this from happening.
Molecular hydrogen acts quickly to stop and even reverse the effects of oxidative stress in the body, and can also reduce inflammation and allergic reactions in the respiratory system. Since interstitial lung disease involves oxidation of the tissues surrounding the lungs (and subsequent scarring and stiffening of these tissues), use of molecular hydrogen administered by nebulization may be able to stop this from happening.
Nebulization delivers particles of a medicine (such as molecular hydrogen) directly into the lungs, which is why the hydrogen should ideally be administered through this medium.
In the treatment of pulmonary fibrosis, use of H2 (molecular hydrogen) can be extremely beneficial. In one study done on rats, hydrogen therapy was shown to reduce lung injury caused by pulmonary fibrosis, and inhalation specifically of molecular hydrogen was shown to produce the following effects:
- Reduced production of Tumor Necrosis Factor alpha (TNF-a); this is a cytokine responsible for the fibrotic reaction in ILD patients, and can cause tissue damage when it is produced in excess quantities.
- Reduced generation of Transforming Growth Factor beta 1 (TGF-b1); this study speculated that TGF-b1 was somewhat responsible for the airway remodeling seen in pulmonary fibrosis, and so reduction of this factor meant that the progression of the disease was more likely to stop or slow down.
- Diminished thickening of the alveolar wall
- Lessened infiltration of inflammatory cells (such as cytokines, like TNF-a)
- Reduced lung structure distortion
- Alleviated fibrillar collagen deposits in the lungs
- Changed genetic expression to reduce expression of genes leading to the development of pulmonary fibrosis; specifically, the ILD expression genes a-SMA, COL1A1, VEGF, and TGF-b were downregulated after the rats received hydrogen therapy.
- Increases glutathione peroxidase (an antioxidant) activity, specifically in the lungs, but ultimately throughout the whole body.
- Reduces oxidative stress (specifically, molecular hydrogen targets oxidants like peroxynitrite and hydroxyl radicals, though it does not targe certain other hurtful oxidant molecules like nitric oxide… it also does not target hydrogen peroxide, so hydrogen peroxide therapy could potentially be used together with molecular hydrogen therapy in certain cases).
According to this particular study, many positive effects were more significant or became noticeable after 8 hours of hydrogen inhalation therapy. The 8 hours were split into 4 sessions of 2 hours each over the course of a 24 hour period with breaks of 2 hours in between each session (so 2 hours of hydrogen therapy, 2 hours break, and then another 2 hours of therapy until there was a total of 8 hours of hydrogen inhalation). This treatment was administered to the rats over the course of 4 weeks. In a different study, the researchers noted that the experimental rats in the study demonstrated no negative effects from receiving molecular hydrogen therapy (and also that they did have positive results).
Oxygen Therapy for Pulmonary Fibrosis
Oxygen therapy is a commonly prescribed treatment for interstitial lung disease (AKA, pulmonary fibrosis). Supplemental oxygen, delivered through a cannula directly into the nostrils, helps saturate the pulmonary fibrosis patient’s blood with oxygen, thus relieving any damage that might be done through having deoxygenated blood, and also improves the productivity of the patient’s breathing. Whereas without the oxygen, the patient may not get very much oxygen since they may be breathing more shallow or less productively, the supplemental oxygen ensures that they are receiving high quality oxygen in higher-than-normal quantities each time they take a breath. Hyper-charging the body with oxygen not only directly addresses the problems that pulmonary fibrosis patients experience, but can also help the body heal when administered correctly.While oxygen therapy is a more conventionally accepted treatment, and may be offered at hospitals in conjunction with other conventional medicines, patients with interstitial lung disease can choose to use oxygen therapy on its own or in combination with other hand-picked natural therapies. There are oxygen “bars” available in most developed countries where it’s possible to breathe supplemental oxygen as an alternative therapy option. Some boutique health clinics (such as those offering IV nutritional therapy) may also have access to supplemental oxygen, or be able to direct you to a provider who offers this independently of other conventional treatments.
It’s likely that if you’ve been to the hospital for pulmonary fibrosis, you’ve already received some oxygen therapy. However, if you’re planning to use it therapeutically (and not have to go to the hospital every time), seeking out a place that will administer you with supplemental oxygen is important. You may breathe oxygen from an oxygen tank, or the oxygen “bar” you go to may use an oxygen concentrator that concentrates and purifies oxygen from the air around you. Either way, the therapeutic benefits are the same.
Supplemental oxygen may be administered simultaneously with molecular hydrogen to enhance the effects of both medicines. Hydrogen helps the oxygen enter the lung tissues and attach itself to hemoglobin in order to more fully oxygenate the body and effectively deliver the oxygen that the lung tissues need to recover.
N-Acetylcysteine / NAC -
N-acetylcysteine, otherwise known as NAC, is a powerful supplement for people with a variety of lung disorders because not only can it help relieve some of the symptoms of lung problems, it can also help treat the root cause of the disease and lead to eventual healing. Like other people with lung disorders, patients with pulmonary fibrosis may benefit from taking NAC.The first thing to know is that NAC is a natural antioxidant. In pulmonary fibrosis, scarring and tissue damage to the lungs tends to occur as a result of oxidative damage, meaning that there are too many Reactive Oxygen Species molecules in the body (there must be a balance of antioxidants and oxidants, having too much of either one can lead to problems). Thus, taking NAC or other antioxidants can help neutralize some of the oxidant molecules, and the damage can be stopped before it starts. In addition, antioxidants can help tissues repair themselves, meaning that any damage to the lung tissues that’s already been done can be reversed (at least to an extent).
One scientific review of NAC treatment for pulmonary fibrosis observed that the patients who received treatment with N-acetylcysteine showed a reduced decline in lung function (meaning that the degree to which their lungs were functional stayed the same longer than patients who did not receive the NAC). In fact, NAC is so valuable for pulmonary fibrosis patients that it has even been prescribed within conventional medical contexts. It may be inhaled or taken orally as a supplement, though the safety of the oral version is notably safer (these supplements can be purchased online, and therefore may be the best choice for people who want to avoid going the conventional route). The safety of NAC is also extremely high with limited side effects.
The most frequently used oral dose of NAC is 600mg taken 3 times per day (equalling a total daily dose of 1800mg of NAC). This amount may be taken for between 3-15 months, or even longer if necessary.

NOW Brand N-Acetylcysteine - 600mg
Vitamin B3 (Niacin/Nicotinic Acid) for Interstitial Lung Disease
Niacin should be taken as niacin/nicotinic acid if it’s being used for the treatment of interstitial lung disease (there are many different kinds of supplemental vitamin B3 available, and these are the ideal kinds to take in this case). Vitamin B3 is extremely helpful for cardiovascular health, and as such, it can help ensure that the capillaries in the lungs remain strong and that they can do their jobs effectively. It also has some other actions in the body, though, that are important specifically for pulmonary fibrosis patients.In one study, a depletion of nicotinamide adenine dinucleotide (NAD) in the lungs may be connected to the development of fibrosis. Niacin is a precursor of NAD, and therefore was considered a potential therapy since supplementation with niacin would raise NAD levels in the lungs and throughout the body. In the study, niacin was shown to reduce elevated hydroxyproline levels, reversed thickening of the alveolar septa (where fibrotic consolidation tends to occur), and diminished accumulations of inflammatory cells in the lung tissues and air spaces in the lungs.
The beginning therapeutic dose of niacin is 3000mg per day, taken in divided doses of 1000mg at three different times during the day. This dose may be increased significantly though according to a person’s needs. Treatment in the study mentioned above (which was done on hamsters) was administered at a dose that would be equivalent to approximately 17,000mg of niacin per day in a human, which although some people may indeed need to take this much, it’s still a high dose of vitamin B3. Start at 3000mg per day and work your way up until you feel a flush. This is the sign that your body is getting enough niacin.

Centella asiatica (Gotu Kola) to Build and Protect Capillaries
Gotu kola, otherwise known as Centella asiatica, is a popular herb in Asian traditional medicine that can help rebuild capillaries and also protect them from further damage. Since collapsed capillaries are often a serious symptom of pulmonary fibrosis, gotu kola can be a valuable herbal supplement to incorporate into a healing protocol to treat this disease.One of the constituents of gotu kola, asiatic acid, is likely the primary medicinal compound responsible for healing in pulmonary fibrosis patients. This substance has the following qualities:
- Anti-inflammatory and antioxidant
- Reduces transformation/production of transforming growth factor-beta 1 (discussed more above in the section about molecular hydrogen for PF)
- Diminishes levels of a-SMA, TIMP-1, Collagen I, and Collagen III, all of which are implicated in the progression of PF
- Down-regulates infiltration of inflammatory cells into the bronchoalveolar lavage fluid
Gotu kola is available in teas, capsule form, tinctures, and as a standardized extract (which may contain higher levels of asiatic acid, and therefore could potentially be a better choice for pulmonary fibrosis patients). Take 50-250mg of the standardized extract, 2-3 times daily, for a period of 6 weeks. Then take a 2 week break and reassess your situation. Only continue using gotu kola if you feel it is necessary and helpful to your healing.
Gotu kola generally should not be taken in children/teenagers younger than 18 years, and should be avoided in women who are pregnant or lactating. People with liver problems should not take gotu kola since it can sometimes have a negative effect on the liver, particularly when taken in high doses for a longer period of time.
If you choose to take gotu kola, take it for 6 weeks, and then take a 2-week break. Ideally, this herb shouldn’t be taken over the long term, though studies into the effects of taking gotu kola for up to one year have shown the plant to be relatively safe even for this period of time.

MSM (Methyl Sulfonyl Methane) Treatment
Methylsulfonylmethane (usually shortened to MSM) is a naturally-occurring sulfur-based compound known for its anti-inflammatory and antioxidant effects in the body. It is closely related to DMSO (dimethyl sulfoxide), and has even been called “crystallized dimethyl sulfoxide” in the past. Like DMSO, MSM can penetrate deep inside tissues in the whole body and has the ability to penetrate cell membranes with ease.Besides having an application in the treatment of respiratory problems like interstitial lung disease, MSM has also been used to effectively treat the following health problems:
- Joint and muscle pain
- Interstitial cystitis
- Allergic rhinitis
- Colitis
- Parasitic infections
- Arthritis
- Liver injury
- Pitting edema
- Seasonal allergies
- Ichthyosis
- Cancer
- And more…
There are a few mechanisms by which MSM might work to treat respiratory disorders like pulmonary fibrosis. Notably, MSM decreases the amount of TNF-alpha and IL-6 (both pro-inflammatory cytokines) in the body, as well as neutralizing potentially damaging oxidant compounds like nitric oxide and superoxide radicals. It also is an anti-fibrotic agent that stops the production of transforming growth factor-beta 1, a factor that is closely tied to the development of pulmonary fibrosis. Two other factors, Type I Collagen and a-SMA are also inhibited through MSM use as a supplement.
Pulmonary arterial hypertension (PAH) has been implicated in the development of some cases of pulmonary fibrosis, or it may develop after pulmonary fibrosis has been diagnosed. There have been studies on the effects of MSM on the reduction of arterial pressure in rats with this condition. The rats in the study were given doses of 100mg, 200mg, or 400mg per kg of MSM daily for 38 days. At the end of the study, cardiopulmonary hemodynamics (the dynamics of blood flow between the heart and the lungs) were improved in the mice treated with MSM, and the right ventricle systolic pressure was decreased with the mean arterial pressure being increased. Overall, the study concluded that MSM is a potentially important therapy for patients with this complication of ILD.
MSM is a very safe medicine, and may be taken in doses of up to 4845.6mg (48.45 g) per day in humans before any signs of toxicity are noted. One study done on the use of MSM to improve seasonal allergies utilized a daily dose of 2.6g of MSM per day over the course of 30 days; many subjects demonstrated improved upper and lower respiratory symptoms after only 3 weeks of administration.
Related Posts:
Resources: