Substance P and Other Substances That Modulate Pain: What You Need to Know
 Physiologically, nociceptors exist in the human body to warn us of actual or impending tissue damage. When nociceptors are activated, people experience pain. Pain that’s caused by injury to tissues often includes immune cell infiltration (to clear cellular debris and promote wound healing) as well as redness, and heat. Administration of local anesthetics like procaine or lidocaine can inactivate that kind of pain that comes from nociception activation.
Many people with chronic pain do NOT have immune cell infiltration or tissue damage occurring anywhere in their body. These people visit the doctor and go through diagnostic tests only to find that there’s nothing wrong with them, per se. Doctors may respond poorly to patients with chronic pain that has no obvious cause, but if you’re one of these patients, just be aware that pain is extremely complex and it requires nuanced education and effort to overcome in some cases. Medical doctors, as a general rule, lack the knowledge and training to address these pain issues. There’s an established and well-recognized relationship between high stress, trauma, and an abnormal histamine response that leads to chronic pain, for example. In order to reign in this histamine response, you’ll need to work with the emotional as well as the physiological components of the pain response to get rid of pain permanently. Doctors are simply not trained to understand emotions and the relationship between emotions and physiology. For the most part, medical doctors look with judgment at the body-mind-emotion connections, even those that have established, scientific roots that are begging to be addressed in modern conventional medicine.
Physiologically, nociceptors exist in the human body to warn us of actual or impending tissue damage. When nociceptors are activated, people experience pain. Pain that’s caused by injury to tissues often includes immune cell infiltration (to clear cellular debris and promote wound healing) as well as redness, and heat. Administration of local anesthetics like procaine or lidocaine can inactivate that kind of pain that comes from nociception activation.
Many people with chronic pain do NOT have immune cell infiltration or tissue damage occurring anywhere in their body. These people visit the doctor and go through diagnostic tests only to find that there’s nothing wrong with them, per se. Doctors may respond poorly to patients with chronic pain that has no obvious cause, but if you’re one of these patients, just be aware that pain is extremely complex and it requires nuanced education and effort to overcome in some cases. Medical doctors, as a general rule, lack the knowledge and training to address these pain issues. There’s an established and well-recognized relationship between high stress, trauma, and an abnormal histamine response that leads to chronic pain, for example. In order to reign in this histamine response, you’ll need to work with the emotional as well as the physiological components of the pain response to get rid of pain permanently. Doctors are simply not trained to understand emotions and the relationship between emotions and physiology. For the most part, medical doctors look with judgment at the body-mind-emotion connections, even those that have established, scientific roots that are begging to be addressed in modern conventional medicine.

Click here to schedule a health coaching session with us.
Substance P is a pain-causing substance that’s produced naturally in the human body. But substance P does many things besides just play a role in the production of pain. Substance P protects beta cells in the pancreas, for example, the cells that are responsible for the production of insulin and it also prevents pancreatic fibrosis and pancreatic cancer from developing. This should give pause to readers who are looking for pain relief for diabetic neuropathy, a type of pain caused by poor insulin production or insulin resistance in the human cells. Substance P plays a role in the prevention and healing of diabetes (both type 1 and type 2), but it also plays a role in pain production and pain relief. Substance P can be targeted for pain relief via histamine and the mast cells. If your pain problems fit the profile of substance P as a potential underlying cause, you might benefit from treatments that mitigate its effects, but substance P may not be the best target for relieving any type of pain that might be coming from chronic stress or severe trauma because the pancreas is the organ that takes the most direct hit in terms of stress and trauma. Reducing substance P may also reduce pain levels, but in reducing the amount of substance P, you also make the pancreatic beta cells and the pancreas as a whole more vulnerable to damage, cancer development, or the production of fibrotic tissue in the pancreas. When immune cells infiltrate damaged tissues, the axon reflex happens. The axon reflex involves neurotransmitter release locally at damaged neuron terminals or at the site of irritated axons and their branches in tissues that have been damaged or irritated. A variety of neuropeptides and pro-nociception mediators create an “inflammatory soup” at the site of injury. This “soup” is not a whole-body experience that impacts the global physiology of the body. Rather, it is a locally induced event at a place on the body where damage has already occurred to tissues. NK1 receptors, which are also known as neurokinin 1 receptors, bind to substance P as well as with other substances. NK1 receptors were originally thought to be the primary mediator of pain when substance P is involved. Substance P has the highest affinity to the NK1 receptors in comparison with other substances that are attracted to these receptors, after all. The NK1 receptors play an important role in pain transmission as well as endocrine and paracrine gland secretion, vasodilation, red blood cell production, wound healing, the permeability of capillaries, neurogenic inflammation, white blood cell trafficking throughout the body, and the modulation of cellular proliferation. When substance P lodges in the NK1 receptors it can alter the physiology of the body in a variety of ways. However, it is not the interaction between substance P and NK1 receptors that matters in terms of the production of chronic pain. NK1 receptors are involved in inflammation, the stress response, anxiety, and depression, but also vomiting and nausea, endocrine and exocrine gland secretions, vasodilation, and smooth muscle contraction. In addition to its pain-causing effects, substance P is also regarded as a mitogen that plays a role in tumor development and metastasis of cancer. Substance P, as noted above, can protect the pancreas specifically from cancer development. The pancreas, in turn, plays a role in cancer metastasis throughout the body and should be regarded as the primary organ involved in the initial development of all types of cancer based on the Trophoblast Theory of Cancer. Everything You Never Wanted to Know About the Treatment of Chronic Pain... and How to Avoid Painkillers That Will Eventually Kill You - BUY HERE!!!
Everything You Never Wanted to Know About the Treatment of Chronic Pain... and How to Avoid Painkillers That Will Eventually Kill You - BUY HERE!!!
Substance P and NK1 Receptor Antagonists: Big Fail by Big Pharma
If we think of the NK1 receptors as the positive polarity of a magnet and substance P as the negative polarity of a magnet, we can use this metaphor to understand the attraction between an NK1 receptor and substance P. Substance P and NK1 receptors are, in fact, very attracted to each other. There is currently no known substance that is able to push substance P out of an NK1 receptor, a so-called NK1 receptor antagonist. Big Pharma spent quite a lot of money trying to develop NK1 receptor antagonists that would have a higher level of affinity for the NK1 receptors than substance P, but they failed on an epic level. None of the NK1 receptor antagonists had any pain-relieving effects and none of them were able to dislodge substance P from the NK-1 receptors successfully.Interestingly, however, though the NK1 antagonists didn’t work to treat pain or inflammation, the NK1 receptor drugs were effective in the treatment of vomiting. As far as Big Pharma and the Consensus Science community, the big fail of NK1 receptor antagonist-drugs in the treatment of pain created some major doubts in terms of the general model and method, the science being used to develop drugs for pain relief. Big Pharma completely botched the theory of substance-P induced NK1 receptor pain and invested a great deal of money into a model that simply didn’t work.
In 2015, a landmark study demonstrated that Mas-related G-protein-coupled receptor / MrgprB2 (in mice) and its human homolog MrgprX2 is activated by substance P. MrgprX2 is another type of receptor that interacts with substance P. This study showed that blocking the NK1 receptor may be insufficient to prevent pain and inflammation caused by substance P, but another study confirmed that the MrgprB2 receptor is only expressed on mast cells and not on the dorsal root ganglion neurons along the spinal cord. After a nerve injury, sympathetic nerve fibers will sprout in the dorsal root ganglia around large diameter neurons. These so-called “sympathetic sprouts” grow to produce “baskets” that act to enhance the experience of pain in a general way. We talk more about this in our discussion about how pain-begets-pain and how to treat this problem to reduce certain chronic pain conditions.
These extra sympathetic, fight-or-flight nerves sprout in the spinal cord (which is where the dorsal root ganglia are located) and they grow to produce nerves that resemble a basket or nests. These excess nerve tissues serve to enhance the sympathetic activity and the transmission of certain types of pain. Earlier we mentioned the idea that procaine or lidocaine can be used to get rid of chronic pain, sometimes permanently, but substance P has given us the opportunity to talk about how the use of locally administered lidocaine or procaine can actually stop these sprouts from turning into baskets or nests in the spinal cord.
By blocking pain transmission using a numbing agent like lidocaine or procaine at the location of pain, sympathetic sprouting can be significantly blocked so as to prevent the development of a serious chronic pain condition. Further, blocking the nerve transmission with procaine or lidocaine prevented excitability of the injured nerve tissues and the spontaneous production of pain for 4 to 5 weeks after the end of an early nerve blockade.
If your chronic pain has been in place for years, that’s no reason to lose hope. If it hasn’t become obvious to you yet that the nervous system grows, changes, and remodels itself constantly, then we can all recognize this fact and be grateful for it right now. This is a good time to talk about dimethylsulfoxide / DMSO as an over-the-counter medication that can help the nervous system (including brain, nerves, and spinal cord) to remodel themselves and yes, also reduce chronic pain.
Click here to learn more about the DreamLight.app, an online guided meditation and brain-entrainment tool.
DMSO for Chronic Pain
Dr. Stanley Jacobs was an M.D. in Oregon who discovered some of the most miraculous benefits of DMSO for the nervous system. This is the FDA-approved medication with the broadest medicinal action of any other approved synthetic medication. It has a toxicity level similar to that of drinking water. You can buy DMSO over-the-counter, but it does require some learning to use it safely for pain control, especially if you’re applying it to the skin. Essentially, you can administer DMSO orally, in drinking water to kill pain as long as you are not taking prescription medications as DMSO potentiates medications. DMSO can potentiate other medicines like herbs or essential oils or it can sometimes alter the effects when combined with other medications. But if you’re using DMSO by itself, it has an excellent safety profile. With learning, DMSO can be quite an important tool in medicine because of its ability to strengthen the effects of certain drugs, allowing a person to administer a much lower dose of certain drugs. Again, there’s learning involved with DMSO to make sure that you don’t produce a combination that could harm you, so take time to learn about this amazing medicine before you begin using it to get rid of chronic pain.Also, regular DMSO (as opposed to low or no-odor DMSO) causes the body to emit an oyster-like odor. If you are at home and you have family members around you, give them all just a drop of DMSO so that they won’t be able to smell your oyster odor if you’re using regular DMSO. Even a tiny dose of DMSO will make it so loved ones who are in your proximity likely won’t be able to smell your treatment as you work to overcome chronic pain.
I’ll start this brief discussion of DMSO by telling you that Dr. Jacobs used this medicine to heal the spinal cord of a patient who had a C5 fracture. Normally a C5 fracture causes death or paralysis from the neck down, but Dr. Jacobs administered high doses of DMSO intravenously to his patient and this patient eventually recovered and walked out of the hospital.
DMSO has also been used to cure or overcome some of the most serious symptoms of Down’s Syndrome. DMSO in large doses has also been used to cure schizophrenia. So you get the idea. DMSO is a powerful medicine for the nervous system.
In terms of chronic pain, DMSO is perhaps most famous for its ability to get rid of arthritis pain while simultaneously curing arthritis, but it can actually be used on many different types of pain. Indeed, DMSO can be used for any rheumatic disorder including fibromyalgia (which might be regarded by some as a type of “rheumatism”) or other chronic pain conditions involving the muscles, joints, or connective tissues. DMSO is a detoxifying medicine and it also relieves pain through its effects on C-type nerve fibers that are involved in the sensation of pain. DMSO slows C fiber nerve conduction velocity even in low concentrations of 5-7%. Higher concentrations of DMSO completely block C fiber conduction at a concentration above 9%.
C-fiber nerves are unmyelinated sensory nerves that transmit information about itch, temperature, “slow” pain or “secondary pain” such as dull ache. These fibers play a role in diabetic neuropathy as well as arthritis and fibromyalgia so treatment with DMSO can be important for these and related disorders. As a nerve blocking agent, DMSO can reduce pain by preventing “sympathetic sprouting” wherein new sympathetic nerve fibers “sprout” from the dorsal root ganglion in response to a strong and prolonged pain response in the body. These sprouts eventually grow into “baskets” of nerves that exist to provide extra pain conduction to the brain. DMSO and other substances like lidocaine can prevent the development of these baskets when these medicines are used regularly. Over time, and with regular use, these medicines can also get rid of extra nerves that have been developed to carry data about pain to the brain.
Substance P and MrgprB2 / MrgprX2 receptors
Mice that lack the MrgprB2 receptor on their mast cells have a higher pain threshold than mice who have this mast-cell receptor on their mast cells. This suggests that substance P causes pain via the mast cells and the Mrgpr receptors.
So substance P interacts not only with the NK1 receptor but also with the MrgprB2 / MrgprX2 receptors to produce pain. NK1 receptor-drugs don’t reduce pain, but recent studies indicate that the interaction between substance P and the MrgprB2 receptor (the MrgprX2 receptor in humans) on mast cells is an interaction that plays a role in pain and inflammation that might be controllable. This is significant, because this discovery takes us back physiologically to histamine, stress, and trauma as the root cause of chronic pain issues.
Again though, when you remove or reduce substance P in the body to try to hack into mast cell behavior, you make the pancreas more vulnerable to stress, trauma, inflammation, and the development of cancer or fibrosis, so substance P is not likely to be the best target for those wishing to overcome chronic pain in a permanent way.
Mast Cells and Pain
Substance P induces histamine secretion via the mast cells. Mast cells are famous for their role in the production of pain and inflammation so it isn’t surprising that we would arrive at a humble mast cell as we explore the topic of pain from any angle. Various neuropeptides, including substance P, can provoke mast cells to release substances that cause inflammation including the following:
- Histamine
- Tumor necrosis factor-alpha
- GM-CSF
- Interleukin-8
- CCL2
- CCL3
- CCL4
- Cytokines
- Chemokines
Neuropeptides including substance P can also increase vascular permeability that promotes pain in both humans and animals. Leaky blood vessels can release toxins into delicate tissues that then become inflamed and painful.
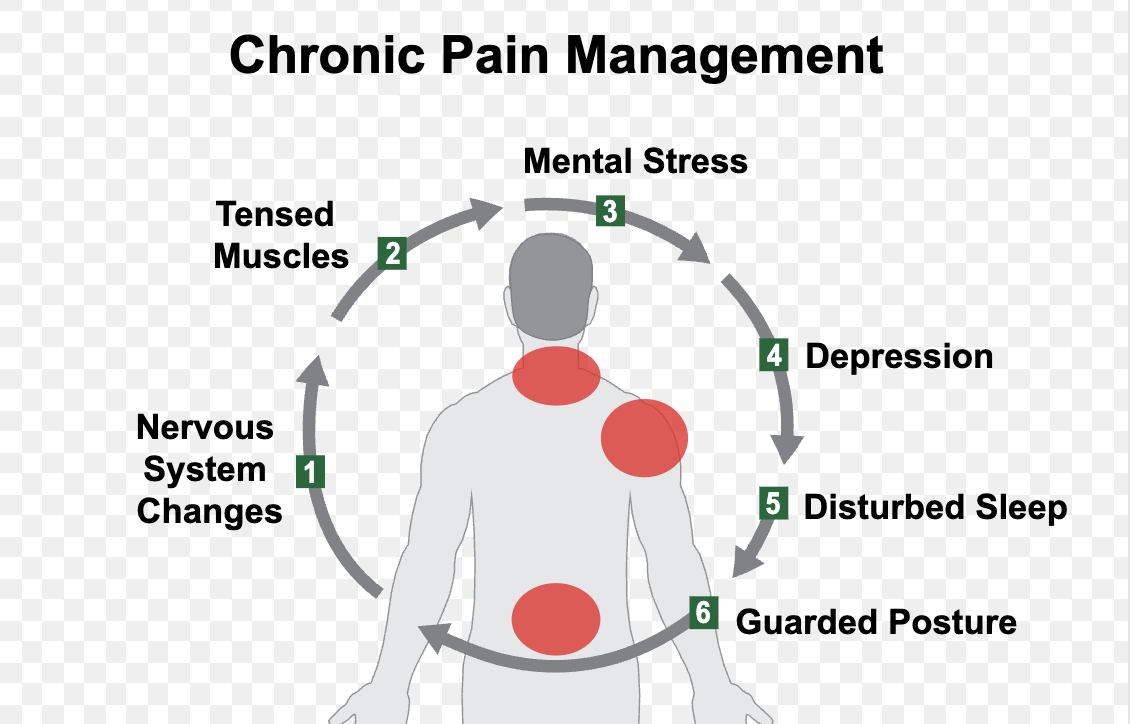
But that being said, mast cells are some of the most important of the first responders in the production of “protective” pain that causes the body to withdraw from intense, possibly damaging environmental stimuli. Mast cells cause pain in order to protect the body from damage. But what if said stimuli were ongoing or so intense that it caused the body to respond with an abnormally high level of adrenaline? Mast cells are located at the interface between the body and the environment on the surface of the skin, in part to play the role of sentinel defense against potentially damaging encounters, but some dangerous or damaging encounters are chronic and debilitating in a way that causes histamine levels to become untethered from adrenaline spikes that normally play a role in spurring the release of histamine. And some of the encounters that we experience as humans with the environment (and with other humans) are so terrifying that the histamine response untethers itself from the adrenaline response in an absolute manner very suddenly. When histamine stops being released as a function of adrenaline release – when histamine is released without the controlling mechanisms of adrenaline to keep it within certain limits – a variety of health issues can develop. One of these health issues is chronic pain, but Mast Cell Activation Syndrome (MCAS), severe allergies, dizziness, digestive issues involving vomiting, and a wide range of other symptoms can develop.
In chronic pain, the proximity of mast cells to nerve endings creates the potential for molecular “cross-talk” between these two cell types. Mast cells take part in “juxtacrine signaling” (as it is called) in the space between neurons and immune synapses. Mast cells can start communicating with nerve endings via histamine release, for example and when this happens, long-term changes in the pain response can take shape.
Remember though, that this is a book about how to alter these kinds of changes in terms of the pain response. Nothing is ever permanent in a body that completely rebuilds and replaces every one of its cells every 7 to 10 years. In order to get the most out of a chronic pain treatment of any kind, it’s important to ride the wave of change and not get stuck on ideas of permanence. The body does a total turnover of all of its cells over the course of 7 to 10 years.
Click here to subscribe to the Living Database now.
We’ve already talked a bit about histamine and pain and the relationship between trauma, high stress, and histamine release and the development of chronic pain, but it’s important to note here that in conventional medicine, the immune system is viewed as its own distinct and separate entity. However, in endobiogeny, the immune system is regarded as a system that is entirely dependent on the autonomic nervous system and the endocrine system to function. In fact, immune system science has coherence, but the nature of immunity in the body is that it is a reactive system. The immune system is not self-regulating. It does not possess its own internal control system, which is good news for lay-readers who are trying to solve their own chronic pain condition. The autonomic nervous system and the endocrine system are much easier systems to understand and work with in terms of treatments and cures. Indeed, these three systems ((immune system, autonomic nervous system, and endocrine system) are regarded in endobiogeny specifically as the same system. What the immune system does is always in response to demands placed on it by the endocrine-autonomic nervous system.Big Pharma funds a great deal of immune system research that very rarely leads to any kind of valuable knowledge that can actually help people in real life to solve their health issues. Studying the immune system to heal the body might be like studying calculus to learn how to make change in a grocery store. So while mast cells technically belong to the immune system (according to conventional medicine), to focus on mast cells is fruitless because they’re reactive and they “freak out”– that’s they’re whole function. Rather, it is much more profitable to focus on trauma-release, stress-reduction, and autonomic nervous system-balancing treatments to begin to be able to control the level with which mast cells are freaking out. In other words, you can’t reason with a mast cell. You can, however, coddle mast cells by releasing stress that’s built up in the autonomic nervous system. Endocrine-balancing herbs and like Garcinia kola and mushrooms like Amanita muscaria provide simple, straightforward treatments for patients to get started at coddling their mast cells. These are treatments that can help a person overcome chronic pain as well as MCAS and other clinical disorders involving the mast cells, but they’re treatment options that take time and that need to be administered consistently over the course of a year or longer to see their full effects.
Clinical pain disorders that are associated with mast cells include the following:
- Migraine headaches
- Pelvic pain
- Bladder pain
- Atopic dermatitis
- Complex Regional Pain Syndrome
- Inflammatory Bowel Pain
- Fibromyalgia
- Self-injurious behaviors due to chronic pain
- Vulvodynia
Scientists have established the fact that pain begets more pain. In other words, if you’re in pain already, stimuli that normally wouldn’t bother you or produce pain will seem more painful than it normally would. A hypersensitivity to pain is hard to understand unless you know a bit about mast cells and the relationship between mast cells, histamine, and nerves that ultimately produces the chronic pain response that plagues so many people today. Mast cells that are freaking out tend to freak out even more when provoked a second time before they have the opportunity to calm themselves down. Also, sympathetic “sprouting” that happens during an initial response to acute pain cause extra nerves to “sprout” at the dorsal root ganglion that create “baskets” of extra pain conduction in those with chronic pain conditions. So pain really does beget more pain. On the other hand, if you treat an initial pain response with a medicine like lidocaine (or DMSO) that can block nerve transmission, these sympathetic “sprouts” of extra nerves never form to perpetuate or increase the pain response.

Become an Expert. Do our Anticancer Video Course Series Online.
Substance P: A Summary
There are a number of substances that have been implicated in the chronic pain response, but histamine and mast cells are some of the most common focal points. Substance P has produced a buzz in the scientific community mostly because Big Pharma wants to produce pain-relievers that won’t accidentally heal the root cause of the pain, namely a hyperactive histamine response and mast cell activation, but in reality, substance P is not a great target for pain control. Mast cells are also not a great target for pain control because of their reactive nature.Readers who are working to overcome chronic pain that might be linked to substance P and mast cell reactions are most likely to benefit from therapies that support the pancreas and that promote the release of trauma and stress along with treatments that target other aspects of the pain response. This kind of treatment is more likely to produce pain-control that eventually becomes permanent. If you suffer from chronic pain, seek out trauma-informed therapies like craniosacral therapy, sacred indigenous medicines like psilocybin and Ayahuasca, Eye Movement Desensitization and Reprocessing / EMDR, alpha-theta therapy, brain entrainment, and guided meditation. Trauma and stress are stored in the autonomic nervous system as unconscious information and emotions that have to be released in order to heal from MCAS, chronic pain, and other mast-cell, histamine-related conditions. In order to overcome these diseases, you have to use a mind-body approach in addition to herbal treatments, at-home treatments to reduce the histamine response, and herbal pain-relievers or neural therapy treatments that actually work well enough that your body will stop having the fear-of-pain response that produces pain. Essentially, your body is producing physical pain so as to distract the body from unconscious emotional pain. In order to stop this cycle and overcome the pain response, you have to address the underlying, unconscious emotional issues and at the same time, work to re-tether the histamine response to the adrenaline-response in the body.

Click here to do a free trial of EMDR to Release Trauma.
Resources: