Iodine Therapy, Thyroid Health, and Gallstones/Gallbladder Health
At first glance, the gallbladder and the thyroid wouldn’t seem to be connected at all. In fact, most people would assume that the function of one would have little to do with the other. But, in reality, the health of the thyroid gland heavily impacts the health of the gallbladder. The thyroid plays a vital role in hormone health and balance, and the gallbladder is sensitive to the presence (or lack thereof) of certain hormones. The gallbladder’s ability to function also can affect thyroid health. In either case, iodine therapy is an important natural treatment for gallbladder issues particularly through iodine’s effects on reproductive hormone levels.How the Thyroid Affects the Gallbladder
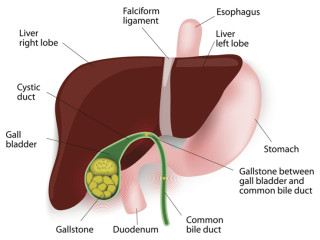
Both hyperthyroidism and hypothyroidism can cause gallbladder problems. Some studies have shown that hyperthyroidism may be slightly more likely to result in the development of gallstones, but hypothyroidism is also a very strong risk factor. One animal study done in 2016 observed that, in a group of rats fed a diet likely to cause the development of cholesterol gallstones, those who had been induced to have hyperthyroidism ALL developed gallstones, 83% of the rats with hypothyroidism developed gallstones, and only 33% of the rats with normal, healthy thyroid function developed gallstones. This link between thyroid function and gallbladder health essentially demonstrates the link between iodine and gallbladder health. Both hypothyroidism and hyperthyroidism are caused by iodine deficiency and/pr a deficiency of one or more of the supporting nutrients involved in iodine metabolism. Click here to learn more about Iodine therapy and the supporting nutrients involved in iodine metabolism.The Sphincter of Oddi, the “gateway” structure that controls the release of bile from the gallbladder into the small intestine, has receptor sites for thyroid hormones. What this suggests, of course, is that thyroid hormones play a direct role in how this gallbladder sphincter works. Therefore, too little or too much thyroid hormone could cause problems not only for the thyroid, but also for the gallbladder, yet another compelling link between iodine sufficiency and gallbladder function (via the general health and functioning of the thyroid gland). Research has shown that too little thyroid hormone ultimately causes a kind of “tension” in this sphincter, making it difficult for it to relax enough to release bile when needed. When bile isn’t released on a normal cycle in normal amounts, it can build up, harden, and eventually develop into sludge or gallstones which can cause upper back pain, frozen shoulder, tennis elbow, headaches, digestive issues, and digestive pain among other things.
Besides actually directly affecting the gallbladder, low thyroid hormone can also slow metabolism which can lead to weight gain as well as digestive issues. A slower metabolism causes the stomach to empty more slowly and less efficiently, which ultimately means bile flow is impeded since without food to digest in the small intestine, bile is not released in the same way. This is another factor that can cause bile buildup in the gallbladder. Initially, this leads to bile “sludge”, but later the sludge can develop into deposits or gallstones.
Finally, the thyroid affects the metabolism of cholesterol in particular. Hypothyroidism specifically can cause higher-than-normal amounts of LDL cholesterol in the body. Since high LDL cholesterol levels are a significant contributing factor in the development of gallstones, it follows logically that problems with the thyroid’s effects on metabolism of cholesterol would ultimately lead to more cholesterol-rich bile salts, and eventually actual gallstones. Indeed, many people who take statin-drugs to treat high cholesterol end up experiencing symptoms of hypothyroidism such as muscle aches and pains (known as statin-related myalgia). Most people take statins to enhance heart health, but through their impact on cholesterol levels in the body, the gallbladder and thyroid gland are negatively affected. And once the thyroid and the gallbladder are affected negatively by statin drugs, other health problems arise such as muscle achiness, weight gain, brain fog, and more. Nonetheless, studies have shown that statin drugs can cause hypothyroidism (or at least symptoms of hypothyroidism even if lab results don't indicate that hypothyroidism is a problem) as well as gallbladder issues.
How the Gallbladder Affects the Thyroid (and How Insulin and Estrogen Connect Them)
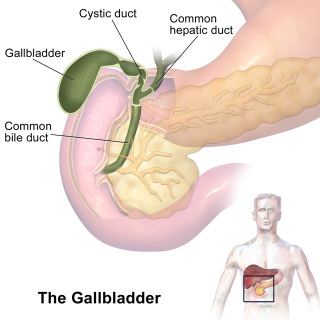
If you really want to understand how the gallbladder’s function affects the thyroid, you first have to know something about the liver and how thyroid hormones are processed and produced in the body. The thyroid hormone known as T4 (thyroxine) is converted into its active form, T3 (triiodothyronine), in the liver. In order to make this conversion, the body must have a sufficient amount of fats. As long as the body is able to process fats adequately during the digestion process, then these thyroid hormones can be produced (this is, of course, a very abbreviated description; the actual conversion process is more complex than this).If the gallbladder has been removed, is blocked, or is otherwise not functioning properly, then the fats that a person eats won’t be digested properly. Bile is required for the breakdown of fats (and thus for the absorption of fatty acids and fat-soluble vitamins, too). If bile is blocked or if its flow is rhythmically “off”, then fat isn’t being digested or absorbed into the body, and the liver won’t be able to convert the T4 hormone into the active T3 form. Inadequate T3 levels lead to a host of problems, one of which is slow metabolism (which, as I discussed above, can ultimately inhibit bile flow as well).
When the body doesn’t have enough T4 in the first place, the liver’s ability to metabolize cholesterol decreases. When this happens, the cholesterol levels in the liver are higher than average, and then subsequently, the cholesterol levels in the bile produced by the liver and stored in the gallbladder are also higher. Higher amounts of cholesterol in the bile increase a person’s risk of developing gallstones since this higher level of cholesterol thickens the bile and makes it more likely to build up in the gallbladder and liver (and also less likely to be excreted properly into the small intestine on cue).
Insulin
When bile flow is abnormal, either due to blockages, low bile production, or other factors, this can lead to insulin resistance. Bile is necessary to keep blood sugar in check, so without sufficient bile flow, blood sugar levels may increase excessively. Bile acids are also required to activate a receptor that can regulate insulin sensitivity. Anyone who has diabetes can benefit from this information which demonstrates the interconnectivity of our organs and systems in the body. The liver, gallbladder, and pancreas are all directly connected via ducts through which both bile and pancreatic enzymes flow. Blockages in these ducts can cause backflow of pancreatic enzymes back into the pancreas where these enzymes can destroy the insulin-producing cells, which leads to diabetes. So here we have a connection between the thyroid gland (and thus, iodine deficiency and/or bromide toxicity) and diabetes via liver health and bile production and flow. Readers who have diabetes who have been diagnosed with thyroid disease can click here to look more closely at liver health, bile and pancreatic supplementation as a cure for diabetes. It’s vital to note once again, however, that Iodine therapy is essential in the treatment of diabetes because of the role that the thyroid gland plays in regulating cholesterol levels and the constituency of bile in the liver and gallbladder. Insulin resistance, as well as either type of diabetes, can affect thyroid health since having too much or too little insulin can ultimately cause problematic changes in thyroid hormone production and action in the body. While this is a somewhat indirect way that the gallbladder affects the thyroid, it’s still a vitally important connection to note in this section. Blood sugar regulation issues, type 2 diabetes, and Hashimoto’s disease (hypothyroidism) tend to co-occur. Gallbladder problems are also extremely common in people who have any one (or all) of these health issues. If you’re looking for a cure for diabetes or a cure for Hashimoto’s disease, it’s important to take liver and gallbladder health into consideration as targets for healing. Click here to read about herbal cures for diabetes that work by regrowing the insulin-producing cells in the pancreas.Estrogen Estrogen is another hormone that connects the gallbladder and the thyroid. The gallbladder (or rather, the bile that it releases) plays a crucial role in estrogen metabolism, meaning that the bile released by the gallbladder is necessary in order to process and regulate estrogen levels in the body. When the gallbladder is sluggish, not producing enough bile, or when there are stones or sludge blocking the gallbladder sphincter, the bile isn’t able to capture and process excess estrogen adequately. This leads to high levels of estrogen. High estrogen levels that may be caused by gallbladder problems can also increase the risk of a sluggish gallbladder, as well as increasing the amount of cholesterol in the body and therefore the potential risk for gallstone development (a downward spiraling effect). In many cases the initial problem begins (and can end) with gallbladder health, or lack thereof although more and more of our clients today develop health issues as a result of receiving bioidentical hormone therapy. When it comes to thyroid health, first you have to be aware that estrogen competes with thyroid hormone for receptor sites. When the body has high estrogen levels, the estrogen can take up sites normally reserved for thyroid hormone. Then, when thyroid hormone comes along to take up residence in those receptor sites, and it finds that they’re already filled with estrogen, it has to keep moving along until it finds a site that’s empty. So this would mean that estrogen is sending out some of the “wrong” signals and the thyroid hormone is unable to do its job effectively. In other words, high estrogen levels can lead to a hypothyroid state. Some of the symptoms of estrogen “dominance” (or an excess of estrogen) include:
- Some of the symptoms of estrogen “dominance” (or an excess of estrogen) include:
- Fatigue
- Low libido
- Irregular or heavy menstruation
- Weight gain
- Hair loss
- Impaired Thinking / Mood Problems
- Depression
- Brain Fog
- Problems with memory
- Sensitivity to the cold, especially cold extremities (like the fingers and toes)
- Bloating
- Tender or swollen breasts
- Fibrocystic breasts
- More severe PMS symptoms
- Headaches
- Panic attacks
- Anxiety
- Insomnia
- Gynecomastia (in men)
- Infertility (in men)
- Erectile dysfunction (in men)
- Fatigue
- Low libido
- Irregular or heavy menstruation
- Weight gain
- Hair loss, brittle hair, and brittle nails
- Impaired thinking / Mood Problems
- Depression
- Brain Fog
- Memory Problems
- Sensitivity to the cold
- Constipation
- Muscle cramps, aches, and weakness
- Carpal tunnel syndrome
Click here to subscribe to the Living Database!
How to Use Iodine Therapy to Treat Thyroid and Gallbladder Problems
Iodine is an important part of gallbladder health since it supports thyroid health (which directly affects gallbladder health, as discussed above). But, it’s also necessary to note that iodine is actually present in fairly high quantities in bile itself. When iodine is taken internally (or put on the skin), it eventually makes its way into the bloodstream. Once in the bloodstream, it then goes to the liver, where it becomes part of bile produced in the liver and then it passes on to be stored and released in the gallbladder. Indeed, gallstones as well as healthy forms of bile both contain iodine, and the iodine levels found in gallstones and bile are lower in people who are deficient in iodine. Some people have suggested that adequate levels of iodine in bile may act as a disinfectant quality in the gallbladder and intestines, as well as potentially playing a role in the prevention of the development of biofilm or a yeast or bacterial infection in these organs as well (specifically, it may help prevent SIBO naturally, a complaint seen very frequently in patients with Hashimoto’s).Iodine therapy is the most important treatment for any thyroid-related problem, including those that affect the gallbladder. This essential nutrient is present in woefully small quantities in most people’s diets, and whatever iodine most people end up eating isn’t able to be used due to an overload of bromide and fluoride from food, water, or other environmental agents (bromine competes with iodine for receptors, leading to iodine deficiency, besides also causing symptoms of fluoride and bromide toxicity). In the US, for example, bromide is ever-present in the water supply throughout the country as a result of bromide-containing insecticide. Fluoride is added to most municipal water supplies. Bromide is sprayed on household products like furniture or children’s pajamas as a “flame retardant”. Bromide and fluoride are often unlisted or sometimes listed ingredients in over-the-counter and prescription drugs. Thus, even if you eat a perfect diet and take care to avoid bromide and other toxins whenever possible, chances are good you’re still getting exposed to bromine / bromide on a daily basis. Click here to read more about over-the-counter and prescription drugs that contain bromine / bromide.
This is why it's essential to take an iodine supplement daily to not only 1) ward off bromide and fluoride toxicity, but also to 2) ensure that you’re getting sufficient iodine to meet the needs of the various organs and glands that need this nutrient.
There are 2 main types of iodine that you can take to combat thyroid and gallbladder problems:
- Lugol’s Iodine 2% - This is a liquid combination of molecular iodine and potassium iodide. You need BOTH of these forms to feed iodine to both the reproductive organs and the thyroid gland. Start by administering 1 drop to your skin or mixed with drinking water taken internally each day. Some people have a strong detox reaction after only 1 drop, while others don’t have much of a reaction at all. As long as you don’t react, increase the dose by 1 drop per day until you reach a dose of 20 drops of the 2% solution each day (1 drop = 2.4 mg). If you have detox symptoms, remain at the dose you’re at until the symptoms go away, and then continue increasing the dose slowly. Keep in mind that Lugol’s Iodine WILL stain clothes and furniture (and will be impossible to get out). It will stain your skin, too, but most of the time it is absorbed relatively quickly by the skin. If you’re worried about having an orange stain on your skin, either rub the iodine into an inconspicuous location on your body, or take it internally in a glass of drinking water. This is the better option for children who can’t take pills, people who are unable to take pills, or individuals who need something lighter on the budget. Lugol’s is also a bit easier to take at a low dose at first if you’re just getting started with iodine.

-
- Iodoral - This is a pill form that combines molecular iodine with potassium iodide, just like Lugol’s Iodine Solution. It tends to be more expensive, but for people who travel a lot or need to have a simpler way to remember their medicines, this might be a better choice (Iodoral is MUCH easier to travel with than Lugol’s Iodine, since you don’t have to worry about it staining/spilling). Iodoral comes in 12.5 mg and 50 mg dosage options. Just like with Lugol’s Iodine, you should start with a lower dose of Iodoral. Start by taking ½ of a 12.5mg pill per day, or even ¼ of a pill if you have a thyroid disorder. Take this dose for a few days, then increase the dose to a ½ pill or a full pill, depending on where you started. For people with thyroid problems or who live in an area with a lot of potential bromine exposure, the goal should be to work up to the 50mg dosage daily, if possible. There may come a time when you can take less than this (such as half of a 50 mg pill only), but start with the goal of working up to a 50 mg dosage. Use the same iodine protocol for Iodoral that we describe at this link for Lugol’s.
This is a safe therapy for anyone of any age or in any situation. Women who are pregnant or lactating, the elderly, and children can all take iodine. Children should receive a lower dose than an adult in most cases. We provide dosage information for adults, pregnant women, babies, and children at this link.
The AlivenHealthy Iodine Bible - Everything you need to know to get started taking iodine and more!
The Barefoot Healer's Guide to Autoimmune Disease, Volume 1 - BUY HERE!
Related Posts: https://alivenhealthy.com/2022/04/24/how-to-use-organic-coffee-and-coffee-enemas-for-gallbladder-and-liver-health/ https://alivenhealthy.com/2022/06/07/castor-oil-packs-an-oil-based-herbal-remedy-for-infertility-reproductive-organ-issues-gallbladder-problems-and-thyroid-disease/ https://alivenhealthy.com/2022/04/24/the-gallbladder-and-the-liver-how-different-systems-of-medicine-view-these-organs-and-their-disorders/ https://alivenhealthy.com/2022/06/11/restoring-libido-by-restoring-gallbladder-health/ https://alivenhealthy.com/2022/02/09/how-to-get-rid-of-gallstones-without-surgery-dr-hulda-clarks-gallbladder-cleanse/ https://alivenhealthy.com/2021/05/13/diarrhea-after-gallbladder-removal-and-how-to-treat-it/ https://alivenhealthy.com/2022/06/05/how-to-correct-nutrient-deficiencies-to-cure-sclerosing-cholangitis/Resources:
 Kelp and seaweed are some of the best dietary forms of iodine.
Kelp and seaweed are some of the best dietary forms of iodine.
 Optimox Iodoral 50 mg Supplement - Potassium Iodide Tablets, High Potency Iodine Tablets, Iodine Supplements for Thyroid Support, Daily Vitamins and Minerals, Lugol's Iodine Solution - 90 Count
Optimox Iodoral 50 mg Supplement - Potassium Iodide Tablets, High Potency Iodine Tablets, Iodine Supplements for Thyroid Support, Daily Vitamins and Minerals, Lugol's Iodine Solution - 90 Count