Overcoming Infertility: Introduction
Female infertility is a complex subject. This article is intended to help clarify the basic causes of infertility in women in order to make the rest of the related content on this site easier to follow and understand. Below we’ve written a brief description of some of the main types and causes of infertility in women, along with some suggestions of cures for these conditions where applicable. Note that Lugol’s iodine and supportive nutrients that promote absorption of iodine is perhaps the most important alternative cure for nearly all of the women’s health issues noted below. There is definitely a pattern in the data regarding women’s health issues, especially during women’s reproductive years, with digestive enzyme therapies showing up a lot as cures for women’s infertility and reproductive organ disease as well.Polycystic Ovarian Syndrome (PCOS)
This condition is by far one of the most common reproductive disorders in women, with between 4-26% of women being affected. Polycystic ovarian syndrome, otherwise known as PCOS, is characterized by the presence of multiple cysts on the ovaries, accompanied by symptoms such as irregular menstruation, heavy periods, pain in the pelvis, hormonal acne, hirsutism (in some cases), and insulin resistance. Many women with PCOS also experience infertility or significant difficulty with becoming pregnant.Lugol’s iodine 2% is a cure for PCOS. Read more about how to cure PCOS naturally using Lugol’s iodine here.
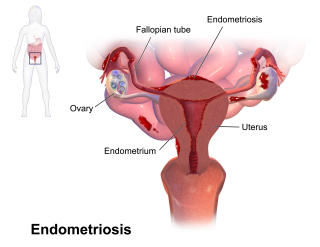
Endometriosis and Endometrial Cancer
Endometriosis is a common female reproductive disorder that affects about 10-20% of women. In other words, it is a common problem for women. In endometriosis, the inner layer of the uterus (the endometrium) begins growing outside of the uterus rather than inside where it belongs. These misplaced endometrial tissues generally grow on the exterior parts of the uterus, fallopian tubes, or ovaries, though in some cases endometrial tissue may begin to grow in other areas of the body as well such as the kidneys, liver, or lungs. Symptoms include pelvic pain, pain during sexual intercourse, heavy menstruation, migraines, gastrointestinal issues, and more. Approximately one-third of women with endometriosis experience infertility. We did a lot of research into this problem to develop a protocol to cure endometriosis as well as endometrial cancer. Click here to read more about this protocol for healing endometriosis naturally.There is an endometriosis-PCOS connection in that both are caused by a deficiency of iodine and both respond well to treatment with Lugol’s iodine (along with supportive nutrients). Lugol’s is a nutrient medicine that combines both molecular iodine and potassium-iodide. Endometriosis and PCOS often co-occur because both are a manifestation of iodine deficiency. Note that the Lugol’s iodine cure for PCOS is also a cure for endometriosis. Read more about the Lugol’s iodine cure for endometriosis and PCOS here.
Additionally, studies have shown that digestive enzymes help tell the endometrium in the uterus to stop proliferating. This data comes from the early 1900s from Dr. John Beard, an embryologist who noted a similarity between the development of a human placenta and the development of a cancerous tumor. To be clear, a human placenta is very different from a cancerous tumor, but one of the main reasons why the endometrium in the uterus does not proliferate out of control in every woman on earth is because excess pancreatic enzymes left over after meal digestion in some women limits endometrial growth. As it turns out, pancreatic enzyme therapy limits endometrial growth. We discuss this idea in depth here in this article about amino acids, enzyme therapy, and fertility diets. Also note that “endo belly” or abdominal pain caused by endometriosis responds very well to enzyme therapy as well.

The AlivenHealthy Iodine Bible - Everything you need to know to get started taking iodine and more!
Premature Ovarian Failure / Premature Menopause
Premature ovarian failure (POF) may also be referred to as primary ovarian insufficiency, premature menopause, or premature ovarian insufficiency. POF is characterized by a significant (if not complete) loss of reproductive/hormonal ovarian function. It is diagnosed only in women under age 40, and is often related to either a dysfunction in the ovarian follicles or the woman’s early loss of all of her eggs. Women with POF experience amenorrhea (loss of menstrual period), estrogen deficiency, and lack of ovarian response to follicle stimulating hormone and luteinizing hormone. The symptoms of this condition resemble those seen in women going through menopause (hot flashes, insomnia, vaginal dryness, decreased libido, etc.).Approximately 5-10% of women may spontaneously restart ovulation after a POF diagnosis without any sort of treatment, conventional or otherwise. This likely occurs in women who accidentally correct an iodine and vitamin K2 deficiency. Read more about how to use Lugol’s iodine and vitamin K2 as a cure for Premature Ovarian Failure / Premature Menopause here. Also note that bee sting therapy, especially when administered to acupuncture points, has been shown to be an effective treatment for premature ovarian failure. Read more about bee sting therapy as a cure for premature menopause / premature ovarian failure here.
Luteal Phase Dysfunction / Luteal Phase Defect
The luteal phase is the period of time after ovulation and before menstruation. It lasts approximately 12-16 days in most women, and during this time, progesterone levels are supposed to increase, while estrogen levels are also supposed to remain consistently high. The increase in progesterone levels during the luteal phases stimulates the growth of the uterine lining in preparation for egg implantation and pregnancy.Women with luteal phase dysfunction may experience a shorter luteal phase than normal or generally decreased progesterone levels. A shorter luteal phase by itself, without any other factors involved, will mean lower-than-normal progesterone levels close to the time of the menstrual period, as well as a thinner (and therefore less viable) uterine lining. Though most women aren’t aware that they have luteal phase dysfunction until the time comes for them to try to conceive, there are some tell-tale signs, such as spotting in between periods and menstruation that regularly comes earlier than expected that may indicate that a woman has luteal phase dysfunction. Having had multiple miscarriages in the past may also point to undiagnosed luteal phase dysfunction.
Parasite infection or a heavy parasite load in the intestines may cause luteal phase dysfunction or metorrhagia (spotting between periods) as well. This is a treatable problem though many women are a bit grossed out by the idea of intestinal worms or parasite infection. Nonetheless, women who are looking for a natural treatment for spotting between periods or fertility issues should consider the possibility that a parasite cleanse is in order. Read more here about menstruation issues and parasites to better understand this issue.
Women with PCOS and/or endometriosis are at a higher risk of having luteal phase dysfunction than other women, as are women with hypothyroidism or hyperthyroidism. Stress, excessive exercise, overeating or undereating and/or being overweight or underweight, and age are all other factors that increase a woman’s risk of luteal phase dysfunction. Once again, the link between thyroid problems and spotting between periods / luteal phase dysfunction points to iodine deficiency. As such, women in search of a luteal phase dysfunction cure need to follow the Lugol’s iodine douche and Castor Oil Pack protocol, which will protect the uterus and treat reproductive organs for parasite infection while simultaneously treating thyroid problems. Read more about the Lugol’s douche treatment here.
Also note that menstrual cycle irregularities like luteal phase dysfunction can sometimes be balanced by using Lunaception, a technique designed to help women sync their cycles with the cycles of the moon (which is the way that nature intended for the menstrual cycle to be).
Pelvic Inflammatory Disease (PID)
Pelvic inflammatory disease (otherwise known as pelvic inflammatory disorder) is caused by an infection present in the uterus, fallopian tubes, ovaries, or pelvis. While there are many different bacteria that may cause PID (and in fact, there are often multiple bacteria that are to blame), Neisseria gonorrhoeae and Chlamydia trachomatis are present in 75-90% of cases. Untreated chlamydia will develop into PID 10% of the time, while untreated gonorrhea develops into PID 40% of the time. Read about how to flush the uterus and clear blocked fallopian tubes with a Lugol’s iodine douche here.While many women are asymptomatic (and therefore may not be aware of their condition until they start trying to conceive), some women do have symptoms, which may include irregular periods, unusual vaginal discharge, lower abdominal pain, pain or bleeding after sexual intercourse, burning sensation during urination, and others. Pelvic inflammatory disease not only can cause infertility, but it can also increase a woman’s risk of experiencing an ectopic pregnancy. Therefore, it’s important for the woman to treat this infection so that she doesn’t experience risks during her pregnancy.
 NatriChlor CD Set w/Accu-Drop Bottles HCL Extra Large Size (8 oz Total)
NatriChlor CD Set w/Accu-Drop Bottles HCL Extra Large Size (8 oz Total)
 Click here to sign up for the CDS Protocols App!
Click here to sign up for the CDS Protocols App!
 Click here to subscribe to the Living Database!
Click here to subscribe to the Living Database!
Incompetent Cervix
Incompetent cervix can also be referred to as weakened cervix. This condition can cause miscarriage (especially in the second trimester) or premature birth, because in women with weakened cervix, the cervical tissues are too weak and the cervix may start to open before it should. While a woman with an incompetent cervix may be able to conceive without issue and the resulting fetus may be perfectly healthy, if the cervix dialtes prematurely, pregnancy loss can occur.
Buy False Unicorn Root tincture here.
False unicorn root is effective in treating incompetent cervix (it is also a powerful herb for threatened miscarriage).Castor oil packs can also be used to treat incompetent cervix and threatened miscarriage.
Stenosis of the Cervix
In uterine cervical stenosis, the endocervical canal (the gateway through the cervix between the vagina and the uterus) is narrower than normal or even entirely closed off. This makes it difficult, if not impossible, for sperm to successfully pass through the cervix into the uterus and into the fallopian tubes where it can then fertilize an egg. Besides causing infertility, in especially severe cases cervical stenosis may partially or complete impede menstrual flow and can cause pain and inflammation in the abdomen known as hematometra due to a backup of blood in the uterus. This may even lead to infection in especially serious cases.Cervical stenosis poses an issue in regard to the entry of sperm into the uterus, and also often affects the cervical mucus. Since the cervical mucus must be hospitable to sperm, this is another way in which cervical stenosis may impact female fertility. Castor oil can help relax muscles and regulate their patterns of contraction, and may work as a cervical stenosis treatment.
Another natural treatment for stenosis of the cervix combines castor oil and dimethylsulfoxide / DMSO, an FDA-approved substance that helps to dissolve scar tissue. If you have stenosis of the cervix due to scar tissue, castor oil and DMSO can be used together to treat this problem.
Click here to read about the medicinal effects of DMSO.
Fallopian Tube Blockage
There are a few different kinds of blockages that may occur in the fallopian tubes:- Hydrosalpinx - In this type of blockage, a fluid blockage occurs near to the ovary; there may also be scar tissue present.
- Proximal tubal occlusion - This occurs when the tubal blockage is located closer to the end of the fallopian tube that connects to the uterus. The blockage may occur as a result of fibroids, endometriosis, mucus plugs, inflammation, or scarring.
- Salpingitis isthmica nodosa (SIN) - This is a type of proximal tubal occlusion associated with endometriosis and/or previous fallopian tube inflammation. SIN is characterized by diverticula along the tubes, and it not only impedes fertility, but also increases the risk of ectopic pregnancy.
Note that blockages may occur in one or both fallopian tubes due to sexually transmitted infection (STI / STD). Castor oil packs (combined with Lugol’s iodine supplementation and DMSO) applied to the abdomen, above the reproductive organs, have been proven to relieve blockages in the fallopian tubes.
Learn more here about how to use Lugol’s iodine in a douche to clear the fallopian tubes if they are blocked.
Uterine Fibroids
Uterine fibroids (which may also be known as leiomyomas) are relatively common, and between 20-80% of women will develop fibroids before the age of 50 when they go through menopause. Fibroids are benign tumors found in the smooth muscle tissues of the uterus, and women diagnosed with fibroids may have only one fibroid, or many, of varying sizes. Many women aren’t even aware that they have uterine fibroids because the fibroids may be too small to cause any adverse health effects, but in some cases, a woman may develop symptoms such as pain during sexual intercourse, chronic lower back pain, the need to urinate frequently, periods that are heavy or notably painful, and anemia.A number of women have developed uterine fibroids as a result of exposure to various brands of hair relaxers that contain phthalates and other endocrine disruptors. Exposure to toxic endocrine disruptors, in this case phthalates, mirrors toxic effects from lead and bromine exposure that women with endometriosis and uterine polyps experience. Lead acetate in hair products for women are just now, at the time of this writing (2022) being removed from circulation despite the fact that people have know about how toxic lead is to women’s health for almost 200 years. Read more here about how lead is still found in cosmetic products, the use of bromine, and how these toxins cause endometriosis as well as other women’s health issues.
Uterine fibroids and endometriosis are related in that both involve an overgrowth of cells. The primary difference between these two diseases is that uterine fibroids are the abnormal growth and out-of-control reproduction of muscle cells while endometriosis is the abnormal growth and out-of control reproduction of endometrial cells. The fact that both of these diseases involve abnormal cellular reproduction makes them both fall into the category of “pre-cancer”, which may sound scary, but in reality, it actually means that women can choose from a wide array of natural cancer cures to overcome these diseases. Read more about cures for uterine fibroids here.
Uterine fibroids can, in about 3% of cases, make it difficult for a woman to conceive a child. When pregnancy is achieved, fibroids also can sometimes increase the risk of miscarriage, premature labor, or bleeding during the pregnancy, and can interfere with the proper positioning of the fetus in the womb.
Though not technically cancerous, uterine fibroids are tumors, and therefore can be treated similarly to uterine or reproductive organ cancers. Alternative medicines such as vitamin B17, iodine, pancreatic enzymes, and Trifolium pratense (red clover) may be especially beneficial for women with uterine fibroids looking to conceive. Castor oil packs have also been used successfully to treat uterine fibroids. Once again, the use of Lugol’s iodine in a vaginal douche along with supportive nutrient therapy can be particularly beneficial for women with uterine fibroids. Read more here about how to use Lugol’s iodine in a vaginal douche.

Click here to buy Trifolium pratense now.
Uterine Polyps / Endometrial Polyps
Uterine polyps are abnormal growths of the endometrial tissue; they are not considered to be tumors in the scientific literature, but rather are more like a skin tag in terms of their pathology. While uterine fibroids are abnormal growths occurring from the muscle cells of the uterus, uterine polyps are abnormal growths emerging from the endometrium or the uterine lining that is shed each month during a woman’s period. In other words, there’s a strong connection between endometriosis and uterine polyps. They are almost synonomous, in fact.Uterine polyps / endometrial polyps are estimated to occur in approximately 10% of women, with many women being entirely asymptomatic. Abnormal uterine bleeding occurs in some cases of uterine polyps, and in situations where a woman experiences this symptom, about 20-30% of the time she will be diagnosed with endometrial polyps. Experts currently disagree as to exactly why uterine polyps can sometimes impede fertility, though they agree that the presence of uterine polyps is correlated often with more difficulty in conceiving.
The treatments that can work to treat uterine fibroids and endometriosis can also be used to treat uterine polyps. These treatments include: vitamin B17, iodine therapy, pancreatic enzymes, and Trifolium pratense (red clover). Once again, a Lugol’s iodine douche can be extremely beneficial for women with uterine polyps. Read more here about how to administer a vaginal douche that contains Lugol’s iodine and water.
Read more about how to cure endometriosis here. The same protocol used to cure endometriosis can be used to cure uterine polyps.
Uterine Adhesions / Asherman’s Syndrome
Uterine adhesions in the reproductive organs, also known as Asherman’s Syndrome, can be caused by previous surgeries (such as Cesarean section), previous infection, or certain diseases of the reproductive organs. Uterine adhesions are areas of scar tissue that have developed and connected two parts of the reproductive organs that aren’t normally connected. Depending on the exact positioning of these adhesions, they may cause infertility by blocking the passage of sperm to the egg, interfering with normal ovulation, or by making it difficult for an embryo to implant appropriately in the uterus.Adhesions sometimes cause blocked fallopian tubes or Asherman’s syndrome (a condition where adhesions form inside the uterus). When adhesions form inside the uterus, this can cause infertility as well as recurrent miscarriage. Symptoms of reproductive organ adhesions can include especially painful menstrual cramps, pain during sexual intercourse, abnormal menstrual bleeding (either too heavy or too light), and amenorrhea. Read more about how to cure Asherman’s syndrome and uterine adhesions here.
Castor oil packs are a proven treatment option for adhesions of the reproductive organs.
Problems with Cervical Mucus
There are different types of problems with cervical mucus that can occur that may interfere with conception, though some are more common than others. For example, a specific type of cervical mucus, which is sometimes known as “egg white” mucus due to the fact that it resembles egg whites in its consistency, is necessary in order for sperm to be able to survive and swim to the uterus and fallopian tubes in order to fertilize an egg.Below are descriptions of some of the issues that can arise with cervical mucus that can impede fertility:
- Antisperm antibodies - These are specific proteins that are produced by the body and that are present in cervical mucus that actively attack sperm that enter the vaginal canal. Of course, this would pose an issue for fertility, since the sperm must be able to live long enough to swim into the uterus and to the fallopian tubes in order to fertilize an egg. Antisperm antibodies may be present if a trauma has occurred to the vaginal mucosa in the past, or if sperm have previously been deposited in the gastrointestinal tract or anus. In addition, if the man has antisperm antibodies in his semen, his partner is more likely to produce them as well.
- Acidic cervical mucus - Cervical mucus that is too acidic is inhospitable to sperm. Ideally, the cervical mucus should be neutral or somewhat alkaline.
- Lack of cervical mucus - A complete lack of cervical mucus can cause vaginal dryness and can make it difficult for sperm to swim in the vaginal canal, through the cervix and into the uterus.
- Cervical mucus that is too sticky/thick - Sticky or overly thick cervical mucus slows down sperm and impedes sperm motility in general.
- Cervical mucus that is too dry - Dry cervical mucus affects sperm motility because it is too sticky or thick, but nevertheless it has a negative effect on sperm mobility. If we compare a single spermatozoa to a fish… when the fish is in regular water, it swims well. If it’s on dry land, it flops about. If you put the fish in syrup or jello, it would have some serious issues being able to swim, if it was able to swim at all. The supplement N-Acetyl-Cysteine (NAC) can be used to thin cervical mucus in order to naturally improve conception rates in women. Read more about NAC as a fertility booster here.
Certain problems with cervical mucus may be caused by hormonal imbalances. However, other factors that can lead to cervical mucus problems include the use of antidepressants, antihistamines, cold and sinus medications, atropine, and other medications, the presence of an infection, cervical damage, or being underweight or overweight. The chances of cervical mucus problems also increase as a woman ages.
As with many of the other women’s health problems, cervical mucus problems can be alleviated with the use of Lugol’s iodine douches and castor oil packs. Read more here about how to use iodine and castor oil to improve fertility naturally.
Lunaception can not only regulate a woman’s actual menstrual cycle, but can also help ensure that the correct type of cervical mucus is produced during ovulation time.
Following an alkalinization protocol with medicines such as aluminum-free baking soda, lithium orotate supplements, or the Budwig Protocol can help cervical mucus be less acidic over time.
Some Traditional Chinese Medicine herbal remedies or treatments such as acupuncture can help control the presence of antisperm antibodies in both men and women. One herbal remedy known as Huzhangdanshenyin has been shown to do just that.
Anovulation
Some causes of infertility are completely unrelated to ovulation, and the woman may still be ovulating normally but still experience problems conceiving. Anovulation is a specific type of infertility where a woman can’t get pregnant because she isn’t ovulating at all. Restarting ovulation is often sufficient for the woman to be able to conceive so long as there aren’t any other factors present that may affect her fertility.Lunaception can help restart ovulation and regulate an irregular menstrual cycle.
Women who are deficient in certain nutrients may stop ovulating because the body knows that the survival of a fetus isn’t possible due to those deficiencies. Lugol’s iodine, again, features heavily into this equation. Read more about how to do the Lugol’s iodine protocol with castor oil packs to restart ovulation.
Poor Ovarian Reserve
Women with poor ovarian reserve may either have low numbers of oocytes left in their ovaries, and/or they may experience problems with oocyte development and recruitment; the quality of remaining eggs may also be impaired in some cases. The condition is often accompanied by unusually high levels of follicle stimulating hormone (FSH). Women who are older are more likely to have this condition, though autoimmune disease, genetic conditions, and previous surgeries or administration of chemotherapy can also sometimes lead to poor ovarian reserve.This health problem is closely related to Premature Ovarian Failure also known as Premature Menopause. As such, women with poor ovarian reserve can work with the same natural treatments for Premature Ovarian Failure that we recommend here.
If you have poor ovarian reserve, your doctor may have recommended IVF. Learn more about the pros and cons of this fertility treatment option here.
Being Underweight and/or Malnourished
Nutrition greatly affects a woman’s ability to get pregnant. When a woman doesn’t have sufficient nutrient stores, and when she isn’t getting enough nutrients in her diet, her body will prioritize her needs first. So even if a chemical pregnancy were to occur, if the woman is malnourished, the pregnancy won’t succeed since the woman’s body will recognize that she doesn’t have enough nutrients to support both her and a growing baby. The same is true if the woman is underweight, since adequate fat stores are essential for a woman to be able to safely carry a baby to term (“safely” referring to both her safety and the baby’s safety, of course).Certain nutrients, such as iodine and vitamin B12 especially, play such a huge role in a woman’s ability to conceive such that if she doesn’t have enough of either one of these nutrients, she’ll experience significant problems with conceiving and carrying a pregnancy to term. Many women with deficiencies in these two nutrients in particular either aren’t able to get pregnant at all in the first place, or they experience multiple miscarriages for no apparent reason. Once a woman begins supplementing with these nutrients, they often have positive results in terms of conceiving a child within a relatively short period of time.
Besides the nutritional factors that play a role in fertility, it’s important to also consider that when a woman is underweight, she won’t produce enough estrogenic hormones. Fat cells produce estrogen, and therefore, if a woman is underweight, she may be estrogen deficient. Women who are overweight risk being estrogen dominant, which can also, in some cases, lead to problems with conception and pregnancy.
Read about nutritional supplements to cure infertility here.
To fully understand the issue of nutrient deficiency that causes infertility, you’ll need to read how certain nutrient deficiencies have been created by governments of the world, particularly in the U.S. to increase profitability in certain sectors of the healthcare system. This may seem very doom-and-gloom, but this context is a reality and it requires mention because women need to be made aware of this issue in order to overcome it. Note that, in all of our content, we seek out hope and treatments to help our readers adapt to the world as it is right now. So, even though we talk a bit about politics and delve into some of the doom-and-gloom, we also provide a wide vista of hope to those who wish to know the whole story. Read about government-sponsored nutrient deficiencies here.
Hypothalamic Dysfunction
The hypothalamus is the starting point for the actions taken by the reproductive organs in the female body; without healthy hypothalamus function, hormonal regulation becomes dysfunctional. Damage to or dysfunction of the hypothalamus affects the pituitary gland directly, which can impair the function of the adrenal glands, ovaries , and thyroid gland. Outside of the pituitary gland, hypothalamic dysfunction negatively impacts oxytocin release, gonadotropin-releasing hormone, growth-hormone releasing hormone, antidiuretic hormone, and corticotropin-releasing hormone.Symptoms of hypothalamic dysfunction may include female infertility, as well as difficulty regulating emotions, sleep disorders, trouble regulating body temperature, changes in growth and weight, and more. It may be caused by any number of things, though stress, genetics, over-eating and/or under-eating, being underweight, and getting too much exercise are all major contributing factors in many cases. The connection between weight and body mass index (BMI) and hypothalamic dysfunction points to an iodine and vitamin K2 deficiency as one of the core causes of this type of infertility.
Read more about how iodine deficiency can lead to weight gain (as well as extreme weight loss via its impact on the thyroid gland).
Also learn more here about government sponsored nutrient deficiencies like iodine and vitamin K2 and how to correct these deficiencies to regain normal fertility levels naturally.
 Nutricost Vitamin K2 MK-7 100 mcg, 240 Softgels - Gluten Free and Non-GMO MK7
Nutricost Vitamin K2 MK-7 100 mcg, 240 Softgels - Gluten Free and Non-GMO MK7
Some women with infertility caused by hypothalamic dysfunction may still release some GnRH in varying amounts, depending on the degree of hypothalamic dysfunction they experience, but regardless, this issue can make a significant impact on a woman’s fertility level.
The hypothalamus is a brain structure that responds well to treatment with amino acids. As such, women with infertility due to hypothalamus dysfunction should read more here about amino acid therapy to boost fertility levels.
Read about how to decalcify the pineal gland (and other brain structures like the hypothalamus) to naturally restore proper reproductive hormone function here.
Maca root is a potential supportive treatment for infertility due to hypothalamus dysfunction.
Hyperprolactinemia
Prolactin is a hormone that isn’t discussed much when it comes to female fertility, but some women may experience an excess of this hormone that can cause infertility. Prolactin is required for breast development, the production of breastmilk after pregnancy, and more. When it is present in excess amounts in women, it can significantly decrease estrogen levels, and may lead to anovulatory infertility as well as irregular menstruation, heavy menstrual flow, galactorrhea (spontaneous production of breastmilk), decreased libido, and breast pain. As hyperprolactinemia impedes the release of GnRH from the hypothalamus, all reproductive hormones and their actions are impeded by the abnormally high levels of prolactin which can cause infertility. In these cases, decreasing the woman’s levels of prolactin is likely to help correct this cause of infertility.Vitex berry is a balancing herbal treatment that can help treat hyperprolactinemia, along with a variety of other fertility-related health issues in women.
Read more about the full protocol detailing how to cure hyperprolactinemia here.
Summary
We’ve selected some of the most common causes of female infertility and researched cures for these health issues to find that many of them share a common treatment, namely Lugol’s iodine and vitamin K2 though other treatments like amino acids and digestive enzymes can also play a role in healing reproductive organ malfunctioning. Many of the herbal remedies for infertility in women contain iodine, vitamin K2, and amino acids, which is why they work so well, but in some cases, herbal treatments contain other vital substances that can assist healing along with the plant consciousness itself.In addition to the fact that Lugol’s iodine therapy plus supportive nutrients is a common treatment for female infertility, it’s also important to note that many reproductive organ problems begin when women are exposed to toxins like phthalates, lead, bromine, fluorine, or organophosphates. Though we don’t talk a lot about organophosphate herbicide and insecticide exposure in this particular article in terms of how these toxins impact fertility, we go into great depth to discuss organophosphate exposure and the health issues caused by herbicides like RoundUp / glyphosate in our book Root Cause, which can be downloaded here.
Read more about how to detoxify your life in a general way to promote fertility here.
Most women who are reading this article are probably suffering from low mood and infertility depression. Treatments that we mentioned above and throughout our book that can be used to naturally get over infertility depression while simultaneously improving fertility levels include Lithium Orotate, Mucuna pruriens, Kudzu, and Lugol's iodine 2% plus the supportive nutrients (to ensure proper absorption of the iodine). Women who are interested in improving fertility while they treat infertility depression naturally should read and follow the endometriosis cure protocol. This is a powerful protocol for healing that can include high pH therapy (using Lithium Orotate in place of Cesium or baking soda), Mucuna, Kudzu, and Lugol's iodine which all powerfully improve mental health and provide a noticeable lift in mood that literally happens within hours of beginning the protocol. Read how to cure infertility depression using the endometriosis protocol here.
The Mucuna pruriens Protocol: Overcome Dementia, Addiction, ADHD, Mood and Mental Health Disorders
Finally, women who are serious about learning how to naturally overcome infertility, should learn more about the testicular tanning protocol that we outline for men. There is no equivalent to testicular tanning in pop culture for women, but women with fertility issues should still consider using the testicular tanning protocol and melanin-based nutrient supplementation to overcome infertility naturally using the sun, vibrantly colored nutrient substances, and shikimate-pathway aminos like L-tyrosine. Learn more about how to do testicular tanning here.
 The Natural Women's Health Guide, Volume 2 - Fertility, Natural Fertility Enhancers, Infertility Treatments, and Natural Libido Boosters - BUY HERE!
The Natural Women's Health Guide, Volume 2 - Fertility, Natural Fertility Enhancers, Infertility Treatments, and Natural Libido Boosters - BUY HERE!
Resources:

 In our Natural Women's Health series, we talk in depth about the natural cures for infertility as well as infertility depression treatments that not only improve mood, but that also boost fertility levels. If you or someone you love suffers from female infertility, be sure to read the entire article to understand the powerful natural treatments that women are using today to overcome doctor-diagnosed infertility that has been dubbed "incurable" or "untreatable" by conventional medicine.
In our Natural Women's Health series, we talk in depth about the natural cures for infertility as well as infertility depression treatments that not only improve mood, but that also boost fertility levels. If you or someone you love suffers from female infertility, be sure to read the entire article to understand the powerful natural treatments that women are using today to overcome doctor-diagnosed infertility that has been dubbed "incurable" or "untreatable" by conventional medicine. QUEEN OF THE THRONES Castor Oil Pack for Liver Kit - Less-Mess, Reusable, Comfort Sleep Fit - Designed by a Naturopathic Doctor (Organic Castor Oil Included)
QUEEN OF THE THRONES Castor Oil Pack for Liver Kit - Less-Mess, Reusable, Comfort Sleep Fit - Designed by a Naturopathic Doctor (Organic Castor Oil Included)
 Low odor DMSO - Dimethyl sulfoxide liquid 3.4 Oz - 100 ml | Pharmaceutical grade ingredient | High purity | Heiltropfen®
Low odor DMSO - Dimethyl sulfoxide liquid 3.4 Oz - 100 ml | Pharmaceutical grade ingredient | High purity | Heiltropfen®
 Vital Nutrients Lithium Orotate | Vegan Supplement to Support Memory and Behavior Health* | 20mg | Gluten, Dairy and Soy Free | 90 Capsules
Vital Nutrients Lithium Orotate | Vegan Supplement to Support Memory and Behavior Health* | 20mg | Gluten, Dairy and Soy Free | 90 Capsules
 Maju Superfoods 4-in-1 Maca Root Capsules, Organic Black, Yellow & Red Roots w Black Pepper Extract for Absorption (120 ct) | Peru Product, Peruvian Powder, Men & Women Supplement, 60,000 mg
Maju Superfoods 4-in-1 Maca Root Capsules, Organic Black, Yellow & Red Roots w Black Pepper Extract for Absorption (120 ct) | Peru Product, Peruvian Powder, Men & Women Supplement, 60,000 mg
 Nature's Way Vitex Fruit, Traditional Menstrual Cycle Support*, Traditional Women's Health Support*, Chasteberry, Vegan, 320 Capsules (Packaging May Vary)
Nature's Way Vitex Fruit, Traditional Menstrual Cycle Support*, Traditional Women's Health Support*, Chasteberry, Vegan, 320 Capsules (Packaging May Vary)