Lyme Disease: A Great Imitator
Lyme disease is known as a “great imitator”, or a disease that can be difficult to identify or diagnose correctly since it resembles such a wide range of other diseases and disorders. On the other hand, some diseases and disorders may be mistakenly diagnosed as Lyme disease as well. In fact, Lyme disease is considered complex enough to diagnose that there’s an entire subset of doctors known as “Lyme Literate Medical Doctors” who are supposed to be trained to identify the subtle differences between Lyme and other diseases. In this section, we’re going to discuss the idea of “differential diagnosis” as well as misdiagnosis of Lyme disease to stretch the imagination a bit into other systems of medicine that aren’t as label-centric as conventional medicine in terms of how they diagnose and treat disease.Differential Diagnosis for Lyme Disease
Differential diagnosis refers to sets of diseases, disorders or health problems that may have similar symptoms and that resemble each other closely. To tell the difference between these differential diagnoses requires a careful eye and knowledge of the (sometimes) tiny differences between two or more conditions in order to make the correct diagnosis. Lyme disease, as I discuss above, is notorious for having a long list of potential differential diagnoses. Below, I discuss some of the most common differential diagnoses for Lyme disease. Unfortunately, many Lyme disease patients are initially misdiagnosed as having one of the diseases below rather than being diagnosed with Lyme disease from the beginning, which means that many patients end up developing untreated chronic Lyme disease. For some people, it takes years or even decades for a doctor to correctly diagnose their condition. If you suspect that you may have Lyme disease, this list of differential diagnoses may help you better determine your health situation.Other Spirochete Bacteria Infections
Leptospirosis
Leptospirosis, also known as Weil’s disease, is a bacterial infection transmitted through fresh water or contact with the urine, blood, or flesh of an infected animal (note that it’s uncommon, however, to be infected by pets or other humans). The infection can cause a wide range of different symptoms, making Leptospirosis difficult to differentiate from certain other diseases in some cases. Some people don’t have any symptoms at all.The onset of Leptospirosis symptoms can occur anywhere between 2 days to 4 weeks, and usually occurs suddenly. Many people recover after taking antibiotics only to have their symptoms return partly or fully a few days after “recovery”. Untreated Leptospirosis infections can lead to the development of meningitis, liver failure, or respiratory distress. The symptoms of Leptospirosis may resemble Borrelia infections, and symptoms the two infections have in common include:
- Fever (the fever is especially high with Leptospirosis) and/or chills
- Headaches
- Rash
- Aching muscles
- Meningitis (both infections cause swelling of the meninges)
- Stiff neck
Other symptoms of Leptospirosis that may or may not resemble those seen in Lyme disease include:
- Jaundice
- Vomiting/diarrhea
- Red eyes
- Abdominal pain
- Sore throat
Infection with Leptospira bacteria has been acknowledged to sometimes be misdiagnosed as Lyme disease (the reverse may be true as well, that Lyme disease is sometimes misdiagnosed as Leptospirosis).
Helicobacter pylori
Helicobacter pylori is another pathogenic spirochete bacteria like Borrelia, Leptospira, and Treponema. Though the symptoms of H. pylori are often definitively gastrointestinal in most cases, the tricky thing with this particular bacteria is that it can appear to be a variety of different gastrointestinal disorders. It’s not always obvious to tell if you have an H. pylori infection, and, much like with other spirochete bacterial infections, an infection with this bacteria is frequently diagnosed as a different health issue, like one of those listed below:- SIBO (Small Intestinal Bacterial Overgrowth)
- Gastritis
- Gastric adenocarcinoma/Gastric cancer
- Gastric ulcers, duodenal ulcers, peptic ulcers, etc.
- GERD (Gastroesophageal reflux disease)
- Low stomach acid
- Heartburn
- Morning sickness/Hyperemesis gravidarum
- Type 2 Diabetes
- Insulin resistance
- Atherosclerosis
- Cardiovascular disease
- Depression/anxiety
- Chronic fatigue
- Idiopathic thrombocytopenia purpura
- Pneumonia
- Rosacea
Syphilis
Also known as the Great Imitator. Researchers have noted that the Treponema pallidum syphilis bacteria are thermophobic and that the bacteria prefer cool temperatures. They have little resistance to high temperatures and survive best at a temperature range between 30-37 degrees Celsius. The temperature preference of the syphilis bacteria has been used to explain why lesions tend to occur in the groin and armpits and other areas of the body that tend to be at a higher temperatures than other areas of the body. Yaws and the Treponema pallidum bacteria has been shown experimentally to be spread via flies, but patients may tend to develop lesions in the vagina, rectum or on the scrotum due to the additional heat in these areas of the body. This fact is not widely known though it was noted in a document that was sponsored by the WHO. In other words, it’s possible for syphilis to be spread through NON-sexual contact. But politically, syphilis patients are stigmatized by the lack of accurate data in the mainstream about how this disease can be spread. Syphilis is an interesting infection both physiologically and politically. Indeed, there are associations (both physiologically and politically) between syphilis and monkeypox that are worth noting. And the fact that syphilis is another Great Imitator also might interest some readers who are trying to better understand Lyme disease. The symptoms that syphilis and Lyme disease have in common include:- Swollen lymph glands
- Fever
- Tiredness/fatigue
- Rash (the syphilis rash usually begins on the palms of the hands or soles of the feet, and then spreads to other areas, but this isn’t always the case; the Lyme disease rash usually presents differently than this)
- Muscle or joint pain, achiness, and/or weakness
- Neurological symptoms, including meningitis, visual problems, and loss of memory (like Lyme disease, the syphilis bacteria can also spread into the nervous system and brain)
- Trouble concentrating
- Cardiovascular symptoms
Symptoms of syphilis that do not resemble Lyme disease include these:
- Sores on the skin, often in the genital area, armpits, or mouth
- Sore throat
Diseases with Symptoms Similar to Lyme Disease
Eczema and Other Differential Diagnosis for Erythema migrans
Depending on the presentation of an Erythema migrans rash caused by Lyme disease, some doctors may misdiagnose the rash as a different condition (particularly if they’re not especially knowledgeable in the symptoms involved in Lyme disease). Eczema is a relatively common misdiagnosis for the Erythema migrans rash, but other potential differential diagnoses include those listed below:- Granuloma annulare
- Ringworm
- Cellulitis
- Insect bites
Bell’s Palsy: Differential Diagnosis for Neurological Lyme Disease / Neuroborreliosis
One of the symptoms of the neurological manifestation of Lyme disease is facial palsy. Weakness or numbness of the facial muscles may also occur in Lyme disease patients. The two conditions look very similar in a lot of cases, and palsy in neurological Lyme disease may even be misdiagnosed as Bell’s palsy sometimes, but there are some key difference between the two that I’ll list below:- In Bell’s palsy, only one side of the face is affected. In contrast, facial palsy caused by Lyme disease may occur on either one or both sides of the face.
- Some experts believe that Bell’s palsy is caused by a viral infection, whereas facial palsy in Lyme disease is caused by the Borrelia bacteria.
- Patients with Bell’s palsy often don’t have any other symptoms other than facial palsy. Lyme disease patients are likely to have facial palsy as well as other symptoms, which may include numbness or weakness in other areas of the body, fever, aching muscles or joints, and other symptoms.
Facial palsy in a Lyme disease patient occurs between 7-21 days after they’ve been bitten by a tick. It’s likely that the patient will also present other signs of infection before the facial palsy occurs, though in some cases, all symptoms including the palsy will set in around the same time. Treatment of facial palsy in any case is something that should be sought out immediately.
Chronic Fatigue Syndrome (CFS) / Myalgic Encephalomyelitis: A Common Misdiagnosis for Chronic Lyme Disease
An initial diagnosis of chronic fatigue syndrome is surprisingly common for patients who suffer from Lyme disease, especially in cases where they have CHRONIC Lyme disease. In fact, the similarity between the descriptions of these two conditions often is (unfortunately) enough to make conventional medicine doctors doubt the existence of chronic Lyme disease in the first place, and diagnose patients with a chronic Borrelia infection with chronic fatigue syndrome instead.Symptoms that both chronic fatigue syndrome (CFS) and chronic Lyme disease share include:
- Severe fatigue/tiredness
- Headaches
- Muscle and/or joint pain
- Dizziness (particularly when the dizziness when going from a seated/lying down position to a standing up position)
- Enlarged lymph nodes (especially in the armpits or neck)
- Post-exertional malaise - This symptoms involves feeling extra exhausted following more intense physical or mental activity
- Sleep problems
Some experts in chronic fatigue syndrome say that CFS is originally set off by a pathogenic infection of some kind. The COVID-19 virus has been noted recently for causing Long COVID, a set of health problems that also resemble CFS. Infection with the Borrelia bacteria may also very well cause the development of CFS (or… one might say that the symptoms of a chronic Lyme infection are simply more or less the same as those seen in CFS. Your choice). In this article, we discuss something known as the Cell Danger Response and a treatment known as Suramin that has been used to cure autoimmune diseases that share the same autonomic nervous system imbalances. And additionally, in this article, we discuss the autonomic nervous system’s involvement in autoimmunity and autoimmune conditions such as Chronic Fatigue Syndrome.
Autoimmune Disease Misdiagnosis for Lyme Disease
Though chronic Lyme disease itself is sometimes categorized as an autoimmune disease, as a “great imitator”, it is often mistaken for other autoimmune diseases. I’ll briefly discuss some of these autoimmune misdiagnoses below.Rheumatoid Arthritis and Other Arthritic Conditions as Lyme Disease Misdiagnosis
Rheumatoid arthritis is one of the most common misdiagnoses for Lyme disease. Many, many people who have been diagnosed with rheumatoid arthritis (RA), have been prescribed conventional RA drugs, and even lived many years of their lives before finally receiving a Lyme disease diagnosis. Some experts refer to Lyme disease as a “trigger” for RA, while others claim that RA is only a misdiagnosis for chronic Lyme disease. In actuality, a large majority of autoimmune conditions (like rheumatoid arthritis) are caused by a dormant infection or colonizing bacteria living in the liver / gallbladder, so whether or not you believe that Borrelia infection is an RA “trigger” or that RA is a misdiagnosis for a Borrelia infection is somewhat irrelevant. No matter which you believe, the possible treatments for the sickness remain more or less the same.Below is a chart comparing some of the most common symptoms of Lyme disease and rheumatoid arthritis:
| Lyme disease / Borrelia spp. infection | Rheumatoid arthritis (RA) |
| Fatigue/Tiredness | Fatigue/Tiredness |
| Stiff neck | Joint stiffness in more than one joint |
| Pain in the joints | Pain/achiness, tenderness, swelling, or stiffness in more than one joint |
| Fever | Fever |
| Weakness | Weakness |
| Headaches | Symptoms on both sides of the body |
| Numbness | Weight loss |
| Shortness of breath | – |
| Lightheadedness | – |
Other autoimmune inflammatory conditions, including the following, have also been misdiagnosed in patients with Lyme disease.
- Psoriatic arthritis
- Bacterial septic arthritis
- Spondyloarthritis
- Ankylosing spondylitis (AS)
- Osteoarthritis
- Polymyalgia rheumatica
Multiple Sclerosis (MS): Lyme Disease Misdiagnosis
Multiple sclerosis, also sometimes referred to as encephalomyelitis disseminata, is an autoimmune demyelinating disease. MS affects the myelin sheaths that cover the nerve cells in the spinal cord and brain, causing debilitating symptoms that sometimes resemble those seen in neurological Lyme disease (AKA neuroborreliosis). Some of these similar symptoms include:- Muscular weakness
- Diminished coordination
- Numbness
- Blurred vision or other vision problems
- Pain
- Chronic fatigue
- Trouble concentrating or remembering things
- Tremors
Approximately 14% of Lyme disease patients are initially misdiagnosed as having multiple sclerosis. Another 2% report having an initial diagnosis of a different neurological disease, such as amyotrophic lateral sclerosis (ALS), Parkinson’s disease, or multiple systems atrophy. Fibromyalgia is another common condition that many Lyme disease patients may be mistakenly diagnosed as having.
Notably, MS has been acknowledged by the conventional medical community as sometimes having its origin in an initial pathogenic infection. The Epstein-Barr virus is a better known infectious trigger in the development of MS, but other infectious pathogens that are acknowledged to cause the onset of MS include Human herpes viruses, Measles morbillivirus (Measles), mumps, or rubella. Vaccinations may also sometimes cause the development of multiple sclerosis. It’s possible therefore that the Borrelia virus may either itself have symptoms that resemble MS, or even that contracting Lyme disease may cause the development of formal MS (perhaps in the presence of a dormant, underlying Borrelia infection).
In any case, if you’ve been diagnosed with a demyelinating disease like multiple sclerosis and then later you received a Lyme disease diagnosis, you should definitely learn more about natural fumaric acid (as opposed to the super-toxic fumaric acid esters that Big Pharma patented as derivatives of natural fumaric acid). Fumaric acid has the ability to cure multiple sclerosis and psoriasis as well as other autoimmune disorders / symptoms through its work on the liver / gallbladder. In our gallbladder book, we talk at length about the connection between fumaric acid and gallbladder / liver health and how fumaric acid treatment is important as a cure for autoimmune disease.
Sjorgen’s Syndrome Misdiagnosis for Lyme Disease
Sjorgen’s syndrome is an autoimmune disease that affects the tear and saliva glands. It may also affect lymphatic health. Some people who previously were diagnosed with a Borrelia infection and then were “cured” by antibiotics may develop the symptoms of Sjorgen’s syndrome and be diagnosed with Sjorgen’s syndrome. Since most conventional medicine doctors don’t acknowledge the possibility of autoimmunity being caused by dormant, hidden, non-testable infections, this isn’t an uncommon situation.Below I’ve listed the common symptoms of Sjorgen’s syndrome in comparison with those of chronic Lyme disease:
| Lyme disease / Borrelia spp. infection | Sjorgen’s Syndrome |
| Fever | Fever |
| Pain and achiness in the joints | Muscle/joint pain |
| Erythema migrans rash | Skin rash |
| Tiredness/fatigue | Tiredness/fatigue |
| Swollen lymph nodes | Swollen lymph nodes |
| – | Dry eyes/mouth/vagina/other mucosal membranes |
| Trouble focusing/remembering things | Memory and focus problems |
| Headaches | Headaches |
| Numbness | Numbness/tingling in some areas |
Dermatomyositis: Lyme Disease Misdiagnosis
Dermatomyositis is a skin-related, inflammatory autoimmune disease. Though it is not one of the most common misdiagnosis for Lyme disease, the symptoms of this autoimmune disease also closely resemble Lyme disease and some people have been documented to receive a misdiagnosis of dermatomyositis. Again, I’ve included a comparison chart below illustrating some of the common symptoms of dermatomyositis that are similar to those seen in Lyme disease patients:| Lyme disease / Borrelia spp. infection | Dermatomyositis |
| Erythema migrans rash | Red/purple skin rash that may be painful or itchy/rough, dry, or even scaly skin |
| General weakness | Muscle weakness (specifically in the neck, back, shoulders, and hips) |
| Fever | Fever |
| Tiredness/fatigue | Tiredness/fatigue |
| Muscle and joint pain | Painful, swollen joints (that are more painful when they are cold) |
| – | Weight loss |
| – | Calcinosis (calcium deposits under the skin) |
| – | Light sensitivity |
| – | Lung inflammation (in adults) |
Systemic Lupus Erythematosus (SLE) as a Lyme Disease Misdiagnosis
The symptoms of systemic lupus erythematosus (SLE) are broad. This autoimmune disease is classified as an inflammatory tissue disease, and can affect not the tissues throughout the body, including those of vital organs like the kidneys, lungs, and brain, as well as the skin, joints, and blood vessels. Lyme disease can cause symptoms that resemble SLE, and thus, some Lyme disease patients are initially misdiagnosed as having developed systemic lupus erythematosus.Some of the comparable, common symptoms of these two diseases are listed below:
- Fatigue
- Sun/light sensitivity
- Arthritic symptoms (aching joints, muscular pain, etc.)
- Heart palpitations
- Rash
- Chest pain
- Problems with memory and concentration
Besides having some symptoms in common, both SLE and Lyme disease frequently have a pattern of remission and “flares”, or times when symptoms worsen. During remission, symptoms may disappear completely or simply be less intense, and during a flare-up, symptoms reappear or worsen. This cyclical pattern that both SLE and Lyme disease have in common adds to the difficulty in telling the two apart in some cases.
Other symptoms of SLE that may or may not resemble those of a Lyme disease infection include:
- Hair loss
- Weight gain
- Swollen ankles
- Blood clotting
- Mouth sores/ulcers
- Eye-related problems (such as dry eyes, rashes on the eyelids, and inflammation of the eyes or area around the eyes)
Other Differential Diagnoses for Lyme Disease
Again, since Lyme disease is a “great imitator”, there is probably a much longer list than the one below of various types of misdiagnosis for Lyme disease that are possible. Nevertheless, below I’ve included a list of some of the more common misdiagnoses that Lyme disease patients have reported receiving:- Vasculitis
- Tendinitis
- Psychiatric disorders
- Tension headaches
- Viral infections
- Thyroid disorders
- Migraines
- Menopausal symptoms
- Diabetes
- Dementia
- Vitamin B12 deficiency
- Gluten sensitivity / Celiac disease (neurological manifestations)
- Raynaud's Syndrome
- Lead poisoning
- Meniere’s disease
- Irritable Bowel Syndrome (IBS)
- Depression
- Relapsing fever (NOTE: Relapsing fever is also caused by Borrelia spp. bacteria, albeit a different species than the one that generally causes Lyme disease.)
- Horner’s syndrome
- Susac syndrome
Common Lyme Disease Co-Infections
There are many different Lyme disease coinfections, including those listed below.- Allergic reaction to the tick
- Babesiosis
- Chronic fatigue syndrome (CFS) **
- Depression **
- Fibromyalgia **
- Human granulocytic anaplasmosis (HGA)
- Leptospirosis **
- Mononucleosis
- Other insect bites
- Reiter's syndrome / Reactive arthritis **
- Rheumatoid arthritis **
- Scleroderma
- Systemic lupus erythematosus (SLE) **
- Tick-borne diseases
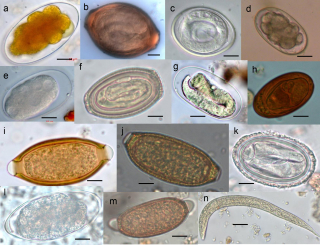
- Parasites
- Viral meningitis **
**These coinfections/accompanying diagnoses are also differential diagnoses for Lyme disease.
Cure Lyme Disease: Scientifically Proven Treatments for Lyme Disease & Co-Infections - BUY NOW!
The Barefoot Healer's Guide to Autoimmune Disease, Volume 1 - BUY HERE!
Related Posts:Resources:

 Areas of the world where Lyme disease is most prevalent.
Areas of the world where Lyme disease is most prevalent.