Natural Cures for Plastic Bronchitis / Bronchitis Fibroplastica
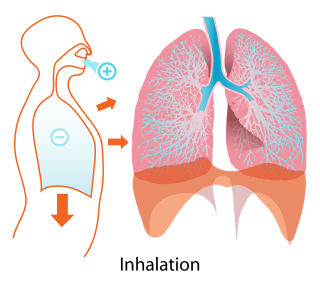
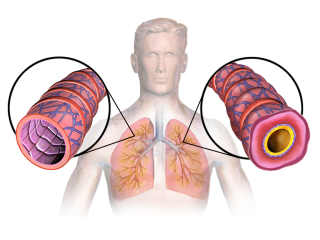
 Plastic Bronchitis (also known as bronchitis fibroplastica) is a rare disease that involves the formation of obstructive “casts” in the bronchial tubes. These casts cause partial or total airway obstruction leading to difficulty breathing. Patients with this disease appear to have an object caught in the airway. Doctors often diagnose the disease when a patient coughs up one of the bronchitis fibroplastic "casts", though this disease can also be diagnosed via bronchoscopy too. Though plastic bronchitis is considered “uncommon”, scientists also acknowledge that it is underdiagnosed and that more patients may have this disease than conventional medicine realizes.
Plastic Bronchitis (also known as bronchitis fibroplastica) is a rare disease that involves the formation of obstructive “casts” in the bronchial tubes. These casts cause partial or total airway obstruction leading to difficulty breathing. Patients with this disease appear to have an object caught in the airway. Doctors often diagnose the disease when a patient coughs up one of the bronchitis fibroplastic "casts", though this disease can also be diagnosed via bronchoscopy too. Though plastic bronchitis is considered “uncommon”, scientists also acknowledge that it is underdiagnosed and that more patients may have this disease than conventional medicine realizes.
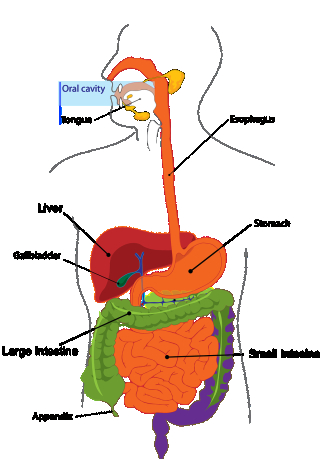
Children often develop plastic bronchitis after they undergo surgery to repair heart abnormalities. The Glenn procedure and the Fontan procedure both increase the risk that a child will develop plastic bronchitis / bronchitis fibroplastica. But this increased risk points to a vital connection between the lungs and the liver via the lymph system that provides a compelling clue in regard to how this disease can be overcome.
 Kid-Friendly Medicines Living Database, BETA Release- NOW AVAILABLE! Click here to sign up...
Kid-Friendly Medicines Living Database, BETA Release- NOW AVAILABLE! Click here to sign up...
There are no pharmaceuticals available to cure plastic bronchitis in conventional medicine, but in alternative and complementary medicine, there’s a different story emerging. Integrative medicine doctors and alternative medicine specialists have discovered that certain systemic and digestive enzymes can be supplemented in patients with plastic bronchitis to cure the disease. Some of the most important enzymes (trypsin and alpha-chymotrypsin) that play a role in curing plastic bronchitis come from the pancreas, an organ that has intimate connection to the lungs. The cure for plastic bronchitis typically involves enzyme therapy with trypsin and alpha-chymotrypsin along with other supportive treatments that we discuss in more detail below. Note, however, that pancreatic enzyme therapy as a stand-alone treatment for cancer has a 13% cure rate (by itself!) in contrast to chemotherapy, which has only a 2-3% cure rate as a stand-alone treatment for cancer. Pancreatic enzyme therapy, as such, has a powerful effect on the body, though they are almost entirely unknown and unused in conventional medicine save for a few doctors who have stumbled across information about supplementing with pancreatic enzymes to restore lung health through their own efforts and research. Nonetheless, pancreatic enzymes are a powerful treatment, but they cause no side effects and they work gently on the body over time. If you have a lung disease, you should take an amylase, lipase, and protease supplement as well as a trypsin and chymotrypsin supplement. Check the ingredients list on the product that you intend to purchase. Many of the pancreatic enzyme supplements do not contain all of these ingredients. You will probably have to buy one product that contains amylase, lipase, and protease and a different product that contains trypsin and chymotrypsin (or alpha-chymotrypsin). Plastic bronchitis is associated with lymphatic anomalies such as malformations in the lymphatic system. This disease brings to light the gut-lymph-lung axis through associations with other diseases like cystic fibrosis, congenital heart disorders, allergic bronchopulmonary aspergillosis, and tuberculosis. Often, plastic bronchitis is seen in patients who have recently had heart surgery, particularly the Fontan procedure, but there we have case studies on file that talk about patients who developed plastic bronchitis following an influenza infection. So the trigger that causes this disease varies from patient-to-patient. It can develop in children as well as adults. The cast formation in plastic bronchitis occurs when the lymphatic anomaly causes an engorgement of the bronchial submucosa. Lymph slowly seeps into the bronchial tubes as a result of this engorgement and then dries out to form the casts. Often, plastic bronchitis remains silent for years and then suddenly manifests in adulthood following a physiological or psychological stressor. As such, plastic bronchitis follows the kind of trajectory that might get it dubbed as an "autoimmune lung disease" by some doctors, but we don't ascribe to the idea of autoimmunity as a concept that has validity because the word "autoimmune" implies that the disease is incurable. And the goal of medicine should be to cure disease. So if the disease name makes patients believe that the disease cannot be cured, then we (Lydian and I) ignore it and look more deeply into the actual underlying cause to find a documented cure in the scientific literature.
 Click here to buy Pancreatic Enzymes.
Click here to buy Pancreatic Enzymes.
Infectious Pathogens Associated with Plastic Bronchitis
Though plastic bronchitis is usually associated with asthma or cystic fibrosis rather than an infectious pathogen in conventional medicine, some patients develop plastic bronchitis in direct relation to an infection such as pneumonia. As a patient, though, you should be aware that infectious pathogens may be the underlying cause of your disease even if you don’t have an active infection that your doctor is able to confirm using conventional laboratory efforts.Many of the so-called “incurable” diseases that seem to have only an “unknown” cause (according to conventional medicine) are actually strongly correlated with pathogens such as:
- Mycoplasma pneumoniae
- Streptococcus pneumoniae
- Influenza, and
- Adenovirus
These pathogens may not be causing an active infection that fits the symptom criteria that doctors normally use to diagnose diseases caused by these pathogens. Rather, they may take up residence and colonize the lymphatic system or other areas of the body (like the liver, for instance) that are hard to reach using conventional medicines like antibiotics that your doctor might prescribe. Patients may not experience the symptoms of infection with these pathogens and instead end up with symptoms that are non-specific that doctors may dismiss as "autoimmunity" or evidence of some other underlying or unrelated disease or disorder.
Scientists and doctors have noted that some patients with plastic bronchitis develop protracted fevers, inflammation, and immune system disturbances. As many readers may already know, autoimmune disorders are often the result of colonizing pathogens that live in remote areas of the body. The lymphatic system is a prime location for colonizing pathogens in part because of its connection to the liver, one of the most important organs involved in autoimmune reactions in the body. In patients with plastic bronchitis, scientists have identified an abnormality in the way the thoracic duct drains from the liver into the lungs. This abnormality is often caused by heart surgery, but it seems like that this "abnormality" may be present for other reasons as well. This discovery is relevant not just to plastic bronchitis, but also other lung conditions as well as congestive heart failure and liver cirrhosis.
The abnormal flow of lymph from the liver into the bronchial tubes is common in plastic bronchitis patients and may be one of the root causes of the disease. Using dynamic contrast-enhanced magnetic resonance lymphangiogram, scientists have been able to show that approximately 94% of patients with plastic bronchitis have lymph fluid draining from the liver via the thoracic duct. They call this abnormal flow of lymph “Abnormal Pulmonary Lymphatic Perfusion”. A surgical procedure to block or embolize the duct is the procedure offered by conventional medicine doctors for this abnormality, but if plastic bronchitis is caused by pathogens in the liver traveling up to the bronchial tubes, this surgery to get rid of plastic bronchitis will only lead to the disease manifesting elsewhere in the body as the lymph fluid re-routes. In other words, if you have an infection / colony of pathogens in an organ, such as the liver, surgery to remove or change the direction or flow of lymph won't get rid of the pathogen. That's logical and most patients can understand that. Surgery will not get rid of a pathogen. If the pathogen is still present in the body, surgery will only weaken the immune system and perhaps change where or how the pathogenic infection manifests.
Reactive Oxygen Species Medicine Cure for Plastic Bronchitis
Plastic bronchitis caused by colonies of pathogens living in the liver or in areas of the lymphatic system that are not able to be reached using antibiotics prescribed by a doctor often can be treated using chlorine dioxide solution (CDS) and dimethylsulfoxide (DMSO). The chlorine dioxide solution is a reactive oxygen species medicine that’s also known as Miracle Mineral Solution (MMS). Dimethylsulfoxide (DMSO), in contrast, mixes with the chlorine dioxide to take it deep into the tissues of the body, including into the lymphatic system and into the liver.There are a number of other reactive oxygen species medicines that can be used to cure plastic bronchitis by killing pathogens that are living in remote areas of the body. Below is a list of other reactive oxygen species medicines that are alternatives to chlorine dioxide solution:
Chlorine dioxide solution has become famous as a cure for chronic lung disease because often, chronic lung disease is caused by infectious microorganisms that are living undetected in areas of the body such as the liver or the lymphatic system. Both chlorine dioxide solution and food grade hydrogen peroxide can be combined with dimethylsulfoxide (a powerful medicine in its own right). Combining a reactive oxygen species medicine such as food grade hydrogen peroxide or chlorine dioxide solution with dimethylsulfoxide helps carry these oxygen-based medicines deep into the tissues (and even into cells) that are being colonized by pathogens. Using a reactive oxygen species medicine with dimethylsulfoxide, patients can treat themselves at home for autoimmune diseases that are caused by colonies of pathogens living in the liver or in the lymphatic system. Reactive oxygen species medicines involves tiny ions and molecules that easily travel throughout the body, but combining a reactive oxygen species medicine like chlorine dioxide solution / Miracle Mineral Solution (MMS) with DMSO potentiates this ability to travel deep into the tissues and also into human cells. Most prescription antibiotic medicines are neutralized by the liver, but reactive oxygen species are not neutralized by the liver. And combining reactive oxygen species medicines with DMSO makes these medicines capable of traveling not just into the liver as an organ, but also into cells to repair damage or to kill viruses that may be replicating inside the cells. Patients who are suffering from plastic bronchitis can self-administer chlorine dioxide solution and dimethylsulfoxide by following the MMS Starting Procedure and then moving on to Protocol 1000 PLUS. For detailed information about chlorine dioxide solution and dimethylsulfoxide, purchase our Chlorine Dioxide Solution (CDS) / Miracle Mineral Solution (MMS) book bundle. These books contain all the information you need to learn how to safely use these two medicines to cure plastic bronchitis.
 Essential Oxygen Food Grade Hydrogen Peroxide, Natural Cleaner, 3% USP, White, 16 Ounce
Essential Oxygen Food Grade Hydrogen Peroxide, Natural Cleaner, 3% USP, White, 16 Ounce
IMPORTANT NOTE: Be sure to do NAC or glutathione nebulizer treatments at least 1 hour after the last chlorine dioxide dose each day and 6 to 8 hours before the next dose of chlorine dioxide to avoid canceling out the effects of the chlorine dioxide treatments.
Trypsin and Chymotrypsin as a Cure for Plastic Bronchitis
Alpha-chymotrypsin is a mucolytic agent which means that it has the ability to liquify mucus and decrease the stickiness of sputum.One case report of an 8 year old child who developed plastic bronchitis as a result of an influenza A infection described a treatment that involved removal of bronchial casts via bronchoscopy. Doctors then instilled alpha-chymotrypsin directly into the child’s trachea. Afterwards, the patient gradually improved and his breathing tubes were removed successfully. But most importantly, at clinical follow-up the child had no symptoms of plastic bronchitis and had not had recurrent casts. In other words the alpha-chymotrypsin acted as a cure for plastic bronchitis in this case.
This case report was likely inspired by a 1962 research article by Bruce and Quinton detailing the use of crystallized trypsin applied topically to digest necrotic debris in the bronchial tubes. This article also talks about the use of crystallized trypsin to liquify thick “exudates” (a substance that has oozed out of the bronchial tubes or lungs). It notes that crystallized trypsin has been used on “numerous occasions” to thin fluid by administering it into the pleural cavity, but after success at administering the trypsin into the pleural cavity, doctors also administered this enzyme as an aerosol to liquify bronchial secretions.
Administration of Trypsin and Alpha-Chymotrypsin as a Natural Treatment for Plastic Bronchitis
Aerosolized trypsin and aerosolized alpha-chymotrypsin have the ability to decrease the viscosity of sputum without damaging living tissues, but oral administration of these enzymes also has a positive impact on sputum viscosity. Indeed, in the early days of enzyme therapy for respiratory disease doctors administered alpha-chymotrypsin and trypsin as intramuscular injections. In the 1960’s, alpha-chymotrypsin (also known as “chymoral”) and trypsin were used to treat the following diseases and disorders:- Bronchial asthma
- Bronchitis
- Sinusitis
- Upper respiratory conditions
A patient with plastic bronchitis can take trypsin and alpha-chymotrypsin supplements at the following dosage: Children: Take 1 tablet containing trypsin 600 USP and alpha-chymotrypsin 600 USP two to four times daily. Adults: Take 2-4 tablets containing trypsin 600 USP and alpha-chymotrypsin four times daily.
Click here to subscribe to the Living Database!
N-Acetylcysteine, Acetylcysteine, or Cysteine: Amino Acid Treatment for Plastic Bronchitis
Case studies have shown that administration of nebulized acetylcysteine is a powerful medicine that can be used to control the symptoms of plastic bronchitis. N-acetylcysteine and acetylcysteine are two additional forms of the amino acid cysteine. N-acetylcysteine and acetylcysteine are the synthetic forms of cysteine. Any of these three forms of cysteine can be used in the treatment of plastic bronchitis.N-acetylcysteine (NAC), acetylcysteine, and L-cysteine thin mucus and have a detoxifying effect on the body that is particularly powerful in terms of liver health. These substances are anti-bacterial and they have the ability to break down biofilm in the lungs and also modulate cytokine synthesis. The thiol group in NAC, acetylcysteine, and cysteine reduces the number of damaging free radicals in the lungs through its antioxidant effects. Interestingly, NAC, acetylcysteine, and L-cysteine also have the ability to normalize glutamate and dopamine transmission in the brain and they are powerful anti-addiction supplements.
 L-Cysteine 1000mg | 100 Powder Capsules | Non-GMO, Gluten Free Supplement | by Horbaach
L-Cysteine 1000mg | 100 Powder Capsules | Non-GMO, Gluten Free Supplement | by Horbaach
How to Administer NAC:
Oral Administration
Patients can take NAC or L-Cysteine in pill form. Below are dosage guidelines for NAC in adults and children with plastic bronchitis: Children: Administer 200 mg three times daily to children 7 years and younger. Adults: Administer 600 mg up to 4 times daily.
 NOW Supplements, L-Cysteine 500 mg with Vitamins B-6 and C, Structural Support*, 100 Tablets
NOW Supplements, L-Cysteine 500 mg with Vitamins B-6 and C, Structural Support*, 100 Tablets
Nebulizing NAC or Glutathione
It is possible to nebulize NAC or glutathione to manage plastic bronchitis at home. Nebulizers are widely available to do these kinds of treatments at home for plastic bronchitis. Below is the recipe that you’ll need to follow to create a glutathione saline nebulizing fluid:Glutathione Nebulizer Treatment:
Purchase a pharmaceutical grade, reduced glutathione product. Put 5mL of nebulizing saline in a glass bowl. Open 1 glutathione pill and add the contents to the saline solution. Mix well. Put the mixture in a nebulizer. Nebulize for 4-5 minutes 1 to 4 times daily.N-Acetylcysteine (NAC) Nebulizer Treatment:
NAC is soluble in water and it can be nebulized as an alternative to using glutathione. Take a capsule of pure NAC (600 mg) and dump it into about ¼ cup of water. Life Extension NAC is a good brand to use for nebulizing NAC. Mix well. Not all of the NAC will dissolve. That’s okay. Using a 3 mL syringe, measure 2 mL into the nebulizing reservoir and nebulize for 4-5 minutes per treatment session. Administer 1-4 treatments daily.Nebulized Saline for Plastic Bronchitis
Children often develop plastic bronchitis as a result of the Fontan procedure or the Glenn procedure (surgeries performed due to heart abnormalities such as hypoplastic left heart syndrome / HLHS, tricuspid atresia, and double outlet right ventricle abnormalities). Doctors working with these children have noted that administering nebulized 3% NaCl solution can be extremely beneficial as an natural remedy for plastic bronchitis.Adults with plastic bronchitis can also benefit from nebulized saline treatments for plastic bronchitis. Though nebulized saline is not a cure for plastic bronchitis, it can help open the airways to improve oxygenation to the other organs of the body and reduce surface tension inside the lungs. If you can open up the lungs to make breathing easier, it may be easier to actually cure plastic bronchitis using the other treatments noted below. Studies have shown that inflammation of the bronchial tubes, which can restrict airflow, is greatly reduced by the use of nebulized saline. Though saline can cause coughing in patients with asthma, after the first 1-10 treatments with saline, most children with asthma can be given nebulized saline at home. If you or your child has a lung disease that involves constriction of the bronchial tubes, ask your doctor if you can try saline nebulization at the office if you’re concerned that nebulizing will cause an extreme reaction that might close the airways.
Both adults and children with plastic bronchitis can benefit from the use of either regular (3%) or hypertonic (7%) saline. Inhalation of 3% or 7% saline has been shown to shorten the course of disease by half in children with pediatric capillary pneumonia. Children with this disease who are given nebulized saline are hospitalized for a quarter of the time required by children with pneumonia who are not given nebulized saline treatments. Indeed, nebulizing saline has been able to increase the cure rate for pediatric bronchiolitis up to 93.7%.
Nebulizing Hydrogen Peroxide for Plastic Bronchitis
Hydrogen peroxide is a Reactive Oxygen Species (ROS) medicine like CDS (Chlorine Dioxide) or Artemisia annua, but unlike these other two medicines, it can be used safely in a nebulizer (you should NEVER nebulize CDS!). Thus, this medicine is a way to deliver ROS directly to the lungs to improve oxygenation of the tissues as well as to kill any infectious pathogens that may be living in the respiratory tract.Hydrogen peroxide 3% solution should be mixed with saline solution to be nebulized. Some ozone therapy practitioners specifically recommend this treatment for all kinds of respiratory issues, including plastic bronchitis. Nebulizing with this combination of hydrogen peroxide and saline solution is safe for people of all ages, including children and infants when administered in smaller amounts. When in doubt, start with a smaller dose and work your way up. Symptoms such as headache, fever, diarrhea, and other flu-like detoxification symptoms are indicative of a dose that’s too high and if you or your child experiences these symptoms after nebulizing, you should reduce the dose. Either lessen the amount of hydrogen peroxide administered during the nebulizer treatments, or shorten the amount of time that you’re using the nebulizer (or even both, if necessary).
To administer hydrogen peroxide nebulizer therapy to treat plastic bronchitis, follow the instructions below:
- Combine 0.1cc of 3% food-grade hydrogen peroxide with 10cc (about 2 teaspoons) of normal saline solution in a glass container. This will make a solution that contains 0.03% hydrogen peroxide. For children, increase the amount of saline solution to 20cc or even 40cc to start to make a less concentrated solution. The maximum tolerable dose (for an adult) is 1cc of 3% hydrogen peroxide in 5cc of saline solution, which would be equivalent to a 0.5% concentration of hydrogen peroxide. Do not go above this dosage for an adult. NOTE: Always use FOOD-GRADE hydrogen peroxide for nebulization. This type of hydrogen peroxide has been chelated and has had heavy metals removed from it, whereas hydrogen peroxide in the pharmacy may contain trace amounts of heavy metals or other toxins. Because you’ll be breathing the H2O2 directly into your lungs, it’s important to use a pure product.
- Add the hydrogen peroxide+saline mixture to the nebulizer reservoir. Store any extra hydrogen peroxide nebulizing solution in a glass bottle in the refrigerator (the extra amount will keep for a few months, but use it fresh if possible).
- Do 4-6 sessions of 10-30 minutes each on the first few days of treatment. If you experience coughing fits, feel short of breath, or have other detox symptoms like those described above, administer the treatment for less time each session to start, and then reduce the number of times per day that you administer the treatment until you’re comfortable and feel more progress than discomfort.
 Essential Oxygen Food Grade Hydrogen Peroxide, Natural Cleaner, 3% USP, White, 16 Ounce
Essential Oxygen Food Grade Hydrogen Peroxide, Natural Cleaner, 3% USP, White, 16 Ounce
- If using 12% hydrogen peroxide, combine ¼ teaspoon of H2O2 with 5 ounces of saline solution to create a 0.1% solution.
- If using 36% hydrogen peroxide, combine ¼ teaspoon of H2O2 with 15 ounces of saline solution to create a 0.1% solution.
- If using 3% hydrogen peroxide, combine ¼ teaspoon of H2O2 with 7 ¼ teaspoons of saline solution.
Also consider these tips for using hydrogen peroxide solution at home:
- If you do not have a nebulizer and cannot get one, instead combine hydrogen peroxide solution with distilled water in a clean, aluminum-free pot (ceramic and stainless steel are good choices) in a 1:5 ratio (so that would be 1 cup of hydrogen peroxide for every 5 cups of water, for example). Cover your head with a towel and create a “tent” over the steam so that you can breathe the steam in deeply. Reduce the dosage by half for children, or even less than this to start, and work your way up slowly.
- If you don’t have access to nebulizing saline solution, try this recipe instead:
- Boil 1 ½ cups of distilled or reverse osmosis water for 20 minutes.
- Pour the boiled water into a sanitized jar with a sanitized lid.
- Before closing the jar, add ½ teaspoon of non-iodized salt and stir until dissolved using a sanitized spoon.
- Wait for the mixture to cool completely (you can put it in the fridge to speed this up) before using as part of a nebulization protocol.
https://alivenhealthy.com/2021/10/27/reactive-oxygen-species-medicine-basic-overview/ https://alivenhealthy.com/2021/11/17/the-small-antiviral-herb-for-covid-encyclopedia-find-an-herbal-cure-for-covid-influenza-the-common-cold-and-more/ https://alivenhealthy.com/2022/05/03/the-lung-disease-family-tree-views-of-lung-disease-from-the-perspective-of-alternative-models-of-medicine/ https://alivenhealthy.com/2019/05/13/pancreatic-enzyme-therapy-dr-kelleys-enzyme-therapy-dr-john-beards-therapy-for-cancer/ https://alivenhealthy.com/2022/05/03/nutritional-deficiencies-and-lung-disease-how-vitamins-and-minerals-play-a-role-in-the-development-of-respiratory-tract-problems/ https://alivenhealthy.com/2022/04/13/a-gentle-but-powerful-cure-for-emphysema-molecular-hydrogen/ https://alivenhealthy.com/2022/03/13/natural-treatments-for-non-cystic-fibrosis-bronchiectasis/ https://alivenhealthy.com/2022/03/11/hypertonic-saline-for-chronic-obstructive-pulmonary-disease-copd-treatment/ https://alivenhealthy.com/2022/04/14/a-cure-for-lung-cancer-treat-lung-cancer-at-home-using-these-remedies/ https://alivenhealthy.com/2022/03/03/natural-cure-for-asthma-lugols-iodine-hormone-balancing-therapy-with-molecular-hydrogen-inhalation-as-a-steroid-inhaler-alternative/ https://alivenhealthy.com/2022/03/02/natural-pulmonary-edema-cures/ https://alivenhealthy.com/2021/11/17/the-small-antiviral-herb-for-covid-encyclopedia-find-an-herbal-cure-for-covid-influenza-the-common-cold-and-more/ https://alivenhealthy.com/2022/05/04/andrographis-paniculata-herbal-cure-for-bronchitis-influenza-chronic-lung-disease-and-more/
Resources:
 AMVILAB Proteolytic Enzymes: Trypsin & Chymotrypsin, Proteolytic Enzymes Supplement, Supports Tissue Health, Reduces Edema & Inflammation Caused by Tissue Injury, Fast Recovery - 60 Capsules
AMVILAB Proteolytic Enzymes: Trypsin & Chymotrypsin, Proteolytic Enzymes Supplement, Supports Tissue Health, Reduces Edema & Inflammation Caused by Tissue Injury, Fast Recovery - 60 Capsules
 Low odor DMSO - Dimethyl sulfoxide liquid 3.4 Oz - 100 ml | Pharmaceutical grade ingredient | High purity | Heiltropfen®
Low odor DMSO - Dimethyl sulfoxide liquid 3.4 Oz - 100 ml | Pharmaceutical grade ingredient | High purity | Heiltropfen®
 Click here to sign up for the CDS Protocols App!
Click here to sign up for the CDS Protocols App! Jiva Botanicals Artemisia Annua Capsules - Sweet Wormwood Supplement - Wormwood Herb Extract from Sweet Wormwood Root - Leverage The Benefits of Wormwood Plant - 90 Capsules
Jiva Botanicals Artemisia Annua Capsules - Sweet Wormwood Supplement - Wormwood Herb Extract from Sweet Wormwood Root - Leverage The Benefits of Wormwood Plant - 90 Capsules
 Pure Encapsulations Reduced Glutathione | Hypoallergenic Antioxidant Supplement to Support Liver and Cell Health* | 120 Capsules
Pure Encapsulations Reduced Glutathione | Hypoallergenic Antioxidant Supplement to Support Liver and Cell Health* | 120 Capsules
 RSV Hypertonic Saline Solution 3% - Nebulizer diluent for inhalators and nasal hygiene devices Helps Clear Congestion from Airways and Lungs – Reduce Mucus (25 Sterile Saline Bullets of 0.17 Fl Oz)
RSV Hypertonic Saline Solution 3% - Nebulizer diluent for inhalators and nasal hygiene devices Helps Clear Congestion from Airways and Lungs – Reduce Mucus (25 Sterile Saline Bullets of 0.17 Fl Oz)