Lung Disease According to Other Models of Medicine
 In this post, we provide a selection of diseases that tend to involve the respiratory system as well as other organs systems of the body to demonstrate how sometimes, lung disease might be rooted in other organs of the body that seem to be completely unrelated to the lungs and respiration. The goal of this chapter is to give patients who are looking for alternative answers to their questions or healers who work with various models of medicine to look at respiratory diseases from a different perspective. We discuss some of the closest and most scientifically studied relationships between the lungs and other organ systems.
In this post, we provide a selection of diseases that tend to involve the respiratory system as well as other organs systems of the body to demonstrate how sometimes, lung disease might be rooted in other organs of the body that seem to be completely unrelated to the lungs and respiration. The goal of this chapter is to give patients who are looking for alternative answers to their questions or healers who work with various models of medicine to look at respiratory diseases from a different perspective. We discuss some of the closest and most scientifically studied relationships between the lungs and other organ systems.
This chapter does not provide an exhaustive list of diseases that involve the respiratory system and other organ systems of the body. Rather, we offer a selection of diseases that co-occur in the lungs and in other areas of the body in the hopes that readers will be able to creatively think about lung disease and solve health problems that may not be responding to typical forms of treatment.
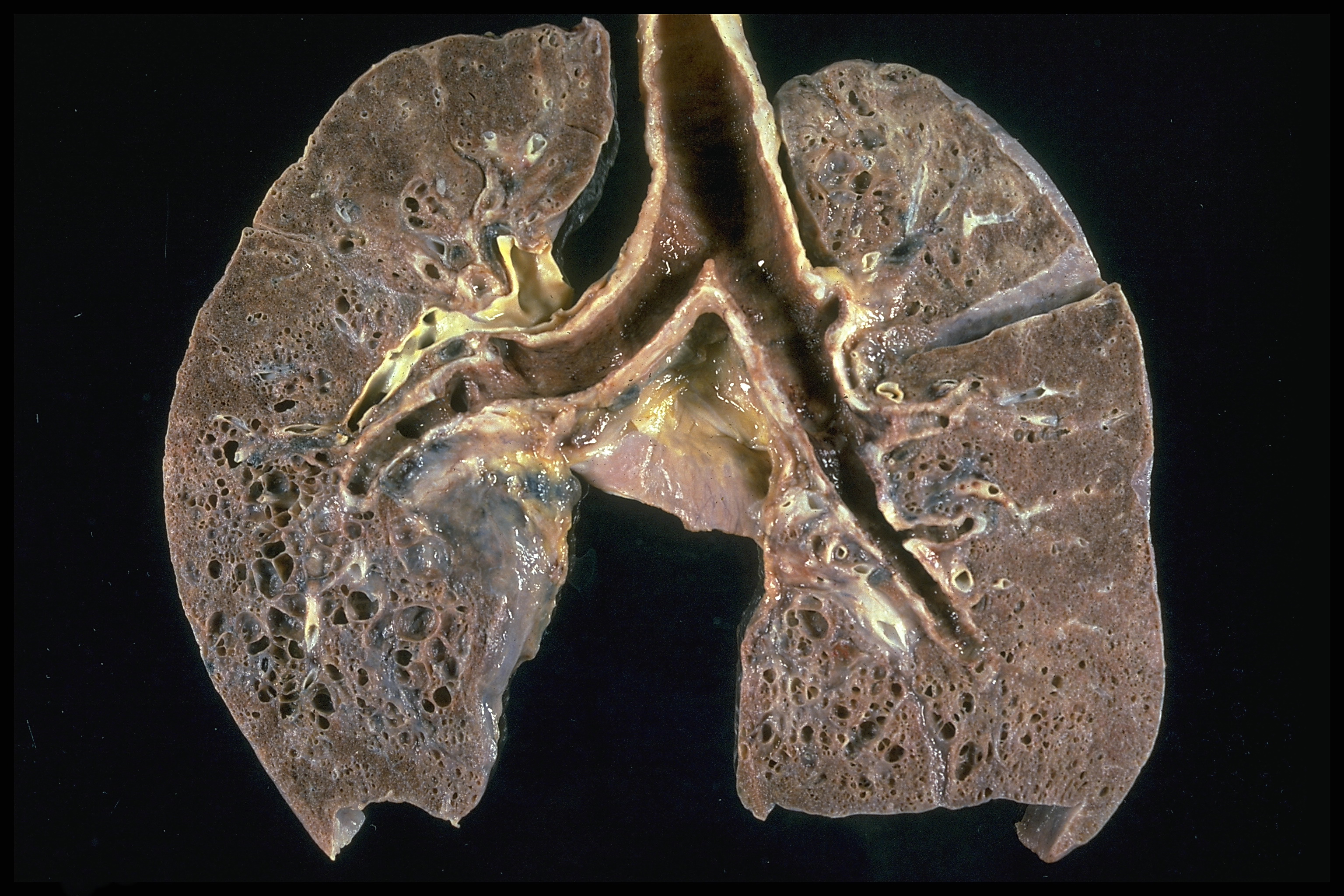
Chronic Lung Diseases
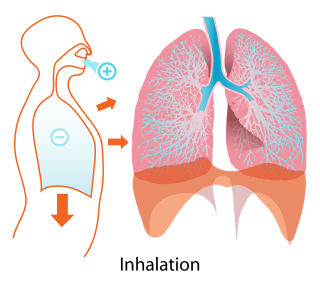
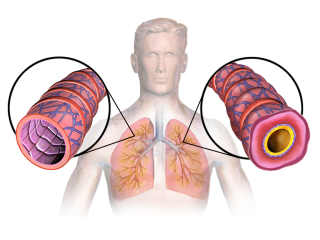
In this section, we’ve listed common chronic lung diseases according to which part of the bronchioles and lungs are most commonly involved in the disease. Note that for many diseases, like emphysema and pulmonary edema, more than one area of the lungs/bronchioles are affected.Chronic lung diseases that affect the airways:
- Asthma
- Chronic Obstructive Pulmonary Disease (COPD)
- Chronic Bronchitis
- Acute Bronchitis
- Emphysema
- Cystic Fibrosis
Chronic lung diseases involving the alveoli:
- Tuberculosis / Mycobacterium tuberculosis
- Pneumonia
- Emphysema
- Pulmonary Edema
- Lung Cancer
- Pneumoconiosis
- Acute Respiratory Distress Syndrome (ARDS)
Chronic lung diseases that affect the blood vessels:
The right side of the heart is responsible for pumping blood into the lungs. The deoxygenated blood travels to the lungs where it becomes oxygenated. The blood travels through the pulmonary arteries into smaller blood vessels in the interstitium to make contact with gases that we inhale such as oxygen and carbon dioxide. The pulmonary arteries or small blood vessels inside the lungs can also play a role in chronic lung diseases such as:- Pulmonary Embolism (Blood clot in the lung) / Deep vein thrombosis
- Pulmonary Hypertension / High Blood Pressure in the Pulmonary Arteries
Chronic lung diseases that affect the interstitium
The interstitium is the thin lining between the alveoli inside the lungs. Blood vessels pass through the interstitium to allow the transfer of gases from the alveoli and the bloodstream :- Interstitial Lung Disease (ILD)
- Sarcoidosis
- Idiopathic Pulmonary Fibrosis
- Autoimmune Diseases
- Pneumonia
- Pulmonary Edema
Chronic Lung Disease and Other Organ Systems in the Body
One of the failings of modern conventional medicine is the way that doctors are taught to divide up the body into different “systems” and then “medical specialities” are created around these systems. For example, if you develop a chronic lung disease, your family doctor is likely to send you to a pulmonologist. This doctor specializes in respiratory system diseases.Though some pulmonologists are knowledgeable about the connection between the respiratory system and other organ systems of the body, often pulmonologists are very focused on just the respiratory system and the drugs and surgeries that are used to cover up symptoms of chronic lung disease. Curing lung diseases like cystic fibrosis or emphysema requires a holistic approach that takes the whole body and all the systems of the body into consideration. Some pulmonologists may have taken the time to study or learn the connection between the respiratory system and other organs of the body, but if not, patients may be prescribed medicines that make the lungs perform better, but that hurt other organs of the body such as the heart or the liver.
Diseases Related to Chronic Lung Disease
In this post we discuss diseases and disorders that are related to chronic lung disease. Or, to put it another way, we will be discussing diseases that are on the same Disease Family Tree with Chronic Lung Disease. There are many models of medicine outside of conventional medicine that take a holistic approach to looking at disease. Traditional Chinese Medicine, for example, looks at connections between different areas and organs of the body. Herbalism also requires knowledge of different plant medicines that are known to work with more than one organ system at the same time. But rather than delving into other famous systems of medicine like Traditional Chinese Medicine or Ayurveda, which can be very technical and alienating for people who were raised under a system of conventional medicine, we are instead providing a discussion regarding diseases (using conventional medicine labels for the diseases) that are related in some way to chronic lung disease.Essentially, we’re using the model of conventional medicine for communication with our readers, but we’re reconfiguring the information to demonstrate that there are valuable insights that can be derived from the patterns that emerge when we look at how different diseases are related to chronic lung disease.
The relationships between chronic lung disease and diseases that are traditionally associated with other organ systems of the body are often fairly well-known by those who suffer from a given lung disease. But by looking closely at these relationships between various diseases in different organ systems of the body, it gets easier to find scientific research and new avenues of thought in regard to cures for chronic lung disease. For example, there is a strong relationship between diabetes mellitus (a disease of the pancreas) and asthma. But this relationship also highlights another relationship between healthy mucus production and pancreatic enzymes. Patients who suffer from plastic bronchitis (wherein “casts” are produced in the bronchials by bacterial infection, causing airway obstructions) for example, can sometimes be cured permanently of their disease by taking trypsin and alpha-chymotrypsin, which are pancreatic enzymes. Indeed, many patients with lung disease who also have diabetes who started taking pancreatic enzymes due to anecdotal reports of efficacy, realized quickly that their diabetes symptoms began to clear up. The results, at times, have been miraculous. And so, patients who suffer either from diabetes mellitus or chronic lung diseases that respond to pancreatic enzyme therapy can gain valuable insights from the scientific research into either of these diseases.
If you’re very serious about finding a cure for a chronic lung disease, using disease family trees can be a valuable tool especially if you tend to think about disease using the conventional medicine model. On the other hand, if you were trained in Ayurveda or Traditional Chinese Medicine or some kind of bodywork, disease family trees might help you better understand your patient’s experience and vocabulary regarding their disease and develop a communication strategy that works better for both of you.
The Pancreas-Lung Connection
As mentioned above, the pancreatic enzymes like trypsin and alpha-chymotrypsin play an important role in healing from a number of chronic respiratory diseases. This connection between the pancreas and the lung became apparent to doctors who work regularly with patients suffering from acute pancreatitis (inflammation of the pancreas that happens suddenly and unexpectedly). The cause of the pancreatic inflammation didn’t matter. In some cases, alcoholism was the underlying cause. More often, gallstones were blocking the pancreatic duct causing a backup of pancreatic enzymes into the pancreas while blocking passage of the enzymes into the digestive system to digest food. In some patients, the pancreatitis had an unknown cause. But in any case, the patients who arrived at the hospital with acute pancreatitis also had various respiratory symptoms.According to one study, patients with pancreatitis also had the following lung and respiratory system issues:
- Hypoxemia (low oxygen levels) - 67%
- Pleural effusion (water on the lungs - a buildup of fluid in the pleural cavity) - 50%
- Atelectasis (lung collapse or closure) - 25%
- Pulmonary infiltrates - 6.7%
- Respiratory failure - 48.3%
Pancreatic disease impacts the lungs through systemic enzymes like trypsin and alpha-chymotrypsin that not only thin mucus, but also play a role in killing bacteria in the lungs and systemically throughout the body via the bloodstream. These digestive and systemic enzymes play a vastly understated role in the prevention of cancer via their circulation in the blood. The exocrine pancreatic enzymes that are released into the digestive system through the common duct that connects the pancreas to the liver and to the gallbladder at the Ampulla of Vater are released into the small intestine at the duodenum, but after digestion is complete, if there are enzymes remaining, they are absorbed into the bloodstream. They then circulate throughout the body in search of cancer cells and pathogens, functioning to dissolve the outer membrane of these cells on an as-needed basis. Eventually, they return to the pancreas where they are recycled and reused. The manufacturing of pancreatic enzymes requires a lot of energy from the body, so recycling these enzymes is valuable and important. Individuals who eat diets that include a lot of meat and animal products may easily use up these enzymes at every meal which taxes the pancreas to produce more enzymes. Of course, some people are able to produce plenty of pancreatic enzymes and they need a diet higher in meats and animal products. But those who are low in pancreatic enzymes may develop a variety of diseases as a result of deficiency.
Pancreatic enzymes such as trypsin, alpha-chymotrypsin, amylase, and lipase circulate in the blood and act as anti-cancer and antibiotic agents. When these enzymes get low, they no longer function to digest pathogenic microorganisms or rogue cells that have taken on a cancerous character. And the lungs are often first in line to suffer the ill effects of pancreatic enzyme deficiency. This is especially true in patients who have had certain types of heart surgery such as the Fontan procedure or the Glenn procedure. Anyone who has a chronic lung disease can probably benefit from pancreatic enzyme supplements that contain alpha-chymotrypsin and trypsin.
Diabetes Mellitus and Chronic Lung Disease
Diabetes is a systemic disease caused by insufficient production of insulin and an abnormal metabolism of nutrients as a result. Without adequate insulin levels, cells have a hard time staying fueled up on natural glucose sugars that they use to stay alive. Diabetes mellitus is not associated with chronic lung disease in popular culture, but there is a strong connection between diabetes mellitus and chronic lung disease via the pancreas in the scientific literature. In other words, scientists are well aware of the fact that diabetes mellitus and lung disease are related diseases.
The connection between asthma and diabetes mellitus is the most solidly established connection in terms of scientific studies that have proven that these two diseases tend to coexist. This connection has been studied most in terms of the blood vessel changes that occur in the lungs when patients develop diabetes mellitus. Blood vessel changes that occur as a result of diabetes can lead to asthma. Indeed, blood vessel changes in the eyes (diabetic retinopathy) is often observed as a problem that mirrors blood vessel changes in the lungs in those with diabetic mellitus.
In diabetes mellitus, the pancreas does not produce enough insulin for one of two reasons. In diabetes mellitus type 1, the beta cells of the pancreas are destroyed in what is typically referred to as an “autoimmune” reaction. In contrast, in diabetes mellitus type 2, the destruction of beta cells is caused by the aggregation of amyloid plaques which are proteins with a specific amyloid shape. This “autoimmune” reaction may be caused by calcification of the pancreas due to a vitamin K2 deficiency.
Studies have shown that patients with diabetes mellitus tend to have more severe lung problems and a more negative trajectory in terms of lung disease. A connection between asthma, COPD, idiopathic pulmonary fibrosis, lung cancer, and pulmonary hypertension has been observed too. And studies have shown that insulin injections tend to make lung diseases worse.
On the other hand, some alternative medicine specialists and integrative medicine doctors who prescribe pancreatic enzyme therapy to patients who have both chronic lung disease and diabetes have seen some miraculous results. The pancreatic enzyme supplements provide support for the pancreas, the organ that is at the core of diabetes mellitus while also providing support for the lungs.
Acanthosis Nigricans
Acanthosis nigricans is a hyperpigmentation of the skin that often happens when patients have high insulin levels like those associated with diabetes mellitus. One case study described the use of fish oil supplements to successfully cure acanthosis nigricans. Though acanthosis nigricans is associated with a variety of illnesses that involve insulin-resistance, one doctor prescribed fish oil to his patient because none of the other pharmaceutical therapies had any effect on the disease. The acanthosis nigricans showed a “striking improvement” within 1 month and completely disappeared within 6 months of fish oil treatments.Interestingly, vitamin K2 is more easily absorbed and used by the body when it is taken with fish oil, which contains an array of the fat-soluble vitamins. Vitamin K2 is a new vitamin that was only recently discovered for its role in ensuring that calcium is placed into bone tissues. Without adequate vitamin K2, calcium is placed in organs and blood vessels causing them to calcify and become diseased. This fact, perhaps highlights the importance of consuming healthy fats in general in the treatment of lung diseases as well as in the treatment of diabetes.
Vitamin D is a fat soluble vitamin that works with vitamin K2. A deficiency of vitamin D can lead to liver disease that causes problems with bile acid production. Bile acid production problems can cause gallstones in the gallbladder and liver duct obstructions that then lead to gut inflammation and gastrointestinal illness.
In other words, these disease states, including diabetes mellitus and acanthosis nigricans (which is often a symptom of diabetes mellitus) are both related to chronic lung disease. In some patients, the relationship between lung disease and pancreatic diseases like diabetes mellitus may be close while in other patients the relationship between these two disease states may seem more distant. If you have diabetes mellitus or acanthosis nigricans with asthma or some other type of chronic lung disease, inevitably these disease states are related through the pancreas and the liver. Enzyme therapy as well as iodine therapy are especially important for those with both lung disease and pancreatic disease.
Vitamin K2 Deficiency and the Calcification of Pancreatic Tissues and Other Soft Tissues
Pancreatic enzyme deficiency plays an important role in a number of chronic lung diseases, but why are patients deficient in pancreatic enzymes in the first place? This is an interesting question that has to do to some extent with diet and nutrition in industrialized nations. Prior to the industrialization of agriculture, animals grazed in pastures on grass. Animals that graze on grass experience a fermentation process in the gut that keeps the animal healthy, but that also causes the animal to produce vitamin K2. The vitamin K2 is a fat-soluble vitamin that is then stored in the animal’s fat to be consumed later by humans.Animals that do not eat grass do not produce vitamin K2 which means that most of the people who are reading this document do not consume vitamin K2 in our diets.
Vitamin K2 works in tandem with vitamin D3 to work with calcium that we consume in our diets. Without vitamin D3, the body won’t be able to absorb calcium properly. But many people today take only a vitamin D3 supplement without vitamin K2 to balance its effects. Unfortunately, vitamin D3 by itself is a vitamin that promotes calcium absorption, but without vitamin K2, this calcium gets placed in soft tissues like blood vessels, organs like the pancreas, the brain, etc. rather than being put where it belongs in bone tissues and teeth.
Vitamin K2 deficiency leads to a number of diseases that develop as a result of soft tissue calcification. Some of these diseases and disorders might surprise you. Erectile Dysfunction (ED), for example, has roots in vitamin K2 deficiency. It’s well-known that ED and cardiovascular problems go together. Indeed, atherosclerosis is another disease that can literally be cured with vitamin K2 supplementation as long as the patient is not taking coumarins or other blood thinning prescription medications that prevent absorption of vitamin K2 and as long as the patient is also not eating trans fats (which also prevent absorption of vitamin K2).
Varicose veins can also be cured by taking vitamin K2 supplements (minus trans fats and prescription blood thinning medications). The role that vitamin K2 plays in revitalizing circulatory system health tells an important story that’s relevant to chronic lung disease because the lungs contain a lot of blood vessels and indeed, without these blood vessels, the lungs would be useless in the body. The lungs, after all, take in oxygen which is then absorbed into the blood. And the lungs expel carbon dioxide which is considered a “waste product” that is collected from the organs by the blood and then deposited into the lung for removal. But there are other substances that are deposited into the lungs by the blood too and the lungs must remove those substances also. Indeed, if the blood supply to the lungs is somehow compromised or if the blood vessels become inflexible or clogged, strange things occur in the lungs. The lungs may fill with fluid, for example. Blood clots in the lungs may occur. So it’s hard to talk about lung health without also talking about vitamin K2 and cardiovascular health.
Trans Fats Antagonize Vitamin K2 and Lead to Calcification of Organs
But in addition to cardiovascular health, the fact that vitamin K2 can cause organs or parts of organs to calcify is an important consideration. This may explain why consumption of trans fats leads to diabetes (perhaps as a result of the calcification of portions of the pancreas that produce insulin) as well as other diseases such as:
- Cardiovascular disease
- Varicose veins
- Breast cancer
- Shortening of pregnancy period
- Heightened risk of preeclampsia
- Nervous system disorders
- Vision problems in infants
- Colon cancer
- Diabetes
- Allergy
- Obesity
Though the lungs are not at the top of the list or organs that are directly affected by the consumption of trans fats or a dietary deficiency of vitamin K2, it isn’t hard to add up the scientific research findings and deduce how the lungs are negatively affected in a serious way via pancreatic affectations since these two organs are so closely connected functionally.
The Lung-Kidney Relationship
The kidneys and the lungs are closely connected in Traditional Chinese Medicine. The lungs and kidneys are related to each other in terms of how they deal closely with the blood. Though all organs must interact with the blood to dump waste and receive fuel and oxygen, the lungs and the kidneys deal with pH level of the blood and both of these organs deal with the removal of waste from the bloodstream.The adrenals, which are situated just above the kidneys, are considered to be the hormonal counterpart of the lungs, perhaps due to their role in regulating the autonomic nervous system via secretion of adrenaline (also known as epinephrine), which in turn regulates the rhythm and depth of our breath.
Scientists have noted that there is definitely a relationship between kidney health and breath, in particular, though this relationship has not been studied as much as it should have been perhaps given the fact that many patients with kidney problems do not respond well to ventilation and the fact that dialysis can cause breathing problems.
Goodpasture’s Syndrome: Kidney Disease and Lung Disease
The kidneys and the lungs are connected in that the kidneys support the activity of the lungs as a person inhales via acid-base balance. In other words, changes in breathing depth or rhythm creates changes in the pH level of the body. To counteract this pH change caused by breath rhythm or depth changes, the kidneys make certain changes to keep pH at a relatively constant level between pH 7.35 and 7.45. In turn, if the kidneys are not functioning properly to maintain pH balance between the narrow range that is optimal in the blood, a patient’s breath may change and become deeper or less often, or more shallow. Because pH levels are so important in regard to health and disease, the lungs and the kidneys work together to keep the acid-base balance within the necessary range.The kidneys are slower than the lungs in terms of their ability to change pH levels in the body. By consciously changing the way that we breathe (in terms of depth and rhythm), we can change our pH levels quickly in the body. On the other hand, if a major pH change occurs as a result of breathing changes, the kidneys can restore the balance, but it takes more time to restore this balance. Thus, the value of breathing variability becomes apparent when we look at the role of breath in maintaining the body’s pH. Scientists have speculated that the reason why patients experience distress after ventilation is because mechanical ventilation does not allow for breath variability.
Goodpasture's Syndrome is a group of illnesses that affect the lungs and the kidneys in patients between 20 to 30 years of age or those who are older than 60 years. It is not as commonly diagnosed in patients between 30 and 60 years of age. In conventional medicine it is considered to be an autoimmune disease because this disease involves antibodies attacking the lungs and the kidneys. Kidney inflammation or glomerulonephritis is a common problem in those with Goodpasture’s Syndrome.
Often, patients with Goodpasture’s Syndrome experience bleeding in the lungs in addition to kidney inflammation. Though the lungs are usually only temporarily affected, the kidneys are often affected long-term.
COPD and Kidney Dysfunction
A variety of diseases co-occur in the lungs and the kidneys. Loss of normal functioning of one of these organs can lead to disorders of the other. COPD sufferers for example, often experience inflammation throughout the body, low oxygenation of the blood, vascular dysfunction, heightened sympathetic nervous system activation, and stiffness in the aorta. The microvascular damage and albuminuria that is part of COPD causes kidney dysfunction. Though often, kidney problems are overlooked in COPD patients, it’s valuable for alternative medicine practitioners to note that both the lungs and the kidneys participate in maintaining the body's pH balance.Pneumonia and Kidney Dysfunction
Chronic kidney disease increases the risk of pneumonia and acute injury to the lungs and acute kidney injury are often associated with complications in critical illnesses. Those with kidney problems are more susceptible to pneumococcal infections. The death rate from pneumonia is much higher among patients with chronic kidney disease, highlighting the value of supporting the kidneys if a patient is ill with a lung disease of any kind.The Gut-Lymph-Lung Axis: How the Gastrointestinal System Affects Respiratory Health (and vice versa)
Though not many people are aware of it, there’s an intimate connection between the well-being of the gastrointestinal system and the well-being of the lungs. When the microbiome of the gut is troubled, this can cause problems with the lungs and respiratory system, or it can sometimes even exacerbate respiratory tract infections like COVID-19, the common cold, whooping cough, or other diseases. Understanding the dynamic between gastrointestinal health and lung health is essential for overcoming many chronic respiratory system problems. Sometimes, the key to resolving a respiratory system issue is in the resolution of problems in the digestive system and the lymphatic system.What is the lymphatic system and why does it matter?
Most people don’t spend a lot of time thinking about their lymphatic system, and because this section involves a discussion of this system, I think it’s important to at least briefly discuss it before moving on to the next part. The lymphatic system plays a vital role in immunity, so it’s important that we give it the attention it deserves.The lymphatic system is part of the immune system and it closely correlates with the circulatory system. The lymphatic system is made up of:
- Lymphatic vessels, which transport lymph through the body
- Lymph nodes, which are responsible for filtering the lymph and targeting infectious pathogens, toxins, or other foreign substances
- Lymphoid tissues, which are present throughout the body, including in the lungs and gastrointestinal organs (such as in the intestines and in the stomach). A function of lymphoid tissue is to help maintain body fluids.
- Lymphatic organs, which include bone marrow (where most lymphocytes are produced), the thymus, and the spleen
Because the lymphatic system is largely responsible for destroying and processing pathogens and other toxins, and because it connects all of the organs of the body, this means that when one organ or organ system suffers, all of the systems end up suffering to some extent. Although western, conventional sensibilities tend to perceive each organ and organ system as its own thing, separate from everything else in the body, the reality is that all of the organs and tissues in the body are connected. Some organs and tissues are more closely related to other specific organs and tissues than others though. In this case, the lymphatic system is a primary link between the gastrointestinal system and the respiratory system.
How the Gastrointestinal System and the Lungs are Connected via the Lymphatic System
The gastrointestinal system and the lungs both have their own distinct microbiome, complete with different kinds of bacteria and microbes that give off different signals to the immune system and other systems that are carried to other parts of the body. When the gut microbiota is healthy and functioning correctly, it sends out signals that decrease inflammation in the whole gastrointestinal system and throughout the body. In contrast, when something is wrong with the gut microbiota, the microbes produce signals that increase inflammation in the body. Poor diet, antibiotics or other medications, pathogens, or other toxins can all interfere with the health of the gut microbiome, and therefore the health of the entire body.The lungs also have their own unique microbiome, similar to the gut, though with fewer microbes and signal-producing bacteria overall. When something goes wrong in the lungs or in the gut with their respective microbiomes, the other is directly affected.
Notably, the gut-associated lymphoid tissue is the most extensive tissue making up the immune system, suggesting that the role of gut health is perhaps one of the most important in terms of fighting bacteria, viruses, and other pathogens. There is also a substantial amount of lymphoid tissue in the respiratory system. Thus, the connection between these two systems via the lymphatic system is very close. Indeed, at the epiglottis, fluids from the respiratory system may flow into the stomach via the esophagus. And fluids from the digestive system could end up in the trachea (and thus, the lungs) if the patient experiences Gastroesophageal Reflux Disorder (GERD), simple indigestion, vomiting, or any other digestive upset that causes digestive juices to move up into the esophagus such that it is able to find its way into the trachea.
The mucosal system works intimately with the lymphatic system. Mucus membranes and the mucus it produces is also an important point of connection between the gut and the lungs. Both the gastrointestinal system and the respiratory system contain mucus membranes that lubricate the organs as needed, protecting against infection, and offering another point of communication between these two systems. Notably, the gut and lungs also develop from the same embryonic tissues and therefore share similar structures. All these points combined make a strong case for the direct and intimate connection between the lungs and the gastrointestinal system.
The microorganisms in the gut (and in the lungs, too) produce both short chain fatty acids (SCFAs) and endotoxins. The SCFAs are primarily responsible for reducing inflammation and inflammatory signals, while endotoxins send out signals that provoke the production of cytokines (such as those seen in cytokine storm syndrome following an infection with COVID-19, for example). When the body is balanced and healthy, more SCFAs are produced than endotoxins, meaning that inflammation is kept in check. But in some cases, more endotoxins are produced (or not enough SCFAs are produced), which can lead to excess inflammation or a cytokine storm in the gut or in the lungs.
The Liver-Lung Connection
Some diseases, like plastic bronchitis, involve a special connection to the liver via the lymphatic system, an important organ associated with the digestive system. The liver is often involved in autoimmune diseases and diseases that seem to be infectious, but that have been deemed incurable by conventional medicine. As an organ of detoxification with extensive ducts that produce bile (a substance that can digests certain types of pathogens, like Streptococcal bacteria for example) the liver plays a central role in controlling many of these “incurable” diseases through both bile production (when bile is being produced normally and in a healthy way), but the liver also acts as an ideal location for pathogens that are colonizing the body.Anyone with a severe disease that seems to be incurable might benefit from supporting the liver and using reactive oxygen species medicines to get rid of pathogens that might be colonizing liver tissues. Antibiotics often aren’t able to reach the liver tissues because the liver filters out the antibiotics or degrades them in such a way that they may not reach liver tissues. Pathogens can then take up residence in the liver and live there quietly until a stressful event occurs or an overpopulation leads to release of these pathogens into the gut or into the lymphatic system.
Though the liver and the lung are normally connected via the lymphatic system even in healthy individuals, there are certain types of heart surgery that can connect the liver and the lungs more directly via the lymph. The Fontan procedure and the Glenn Procedure are two types of heart surgery in children that can lead to a more direct connection between the lungs and the liver via the thoracic duct.
Plastic Bronchitis and Unnatural Lymph Connections Between Liver and Lungs
Children who have had heart surgeries like the ones noted above often develop abnormal lymph flow through the thoracic duct between the liver and the lungs. This abnormality may explain how and why the “casts” develop in the lungs. Some experts believe that the casts that develop in the lungs of patients with plastic bronchitis is due to the presence of bacteria that may be colonizing the liver.Interestingly, however, doctors have used pancreatic enzymes to overcome the problem of casts in certain patients with plastic bronchitis. In some cases, doctors put alpha-chymotrypsin directly into the bronchial tubes of patients with this disease. One dose of alpha-chymotrypsin administered directly into the bronchial tubes can be enough to cure the plastic bronchitis permanently according to case studies. But many doctors are unfamiliar with this procedure. Patients who wish to take high dose trypsin and alpha-chymotrypsin supplements orally, however, experience results similar to the administration of alpha-chymotrypsin directly into the bronchial tubes.
Because some patients with chronic lung disease may be struggling with colonies of pathogens originating in the liver, ox bile supplementation is recommended to help reduce gallstones in the liver and to keep bile moving. Bile helps kill and break down pathogens fully, but if bile flow is impeded, pathogens that wouldn’t normally be able to survive in or near the liver may find a habitable place to thrive. Indeed, psoriasis patients develop skin outbreaks due to low bile flow and the incomplete digestion of Streptococcal bacteria into peptidoglycans which causes leaky gut and attempts by the body to purge the irritating peptidoglycan bits from the bloodstream through the skin.
In addition to the habitable qualities of the liver for pathogens that need a safe place to hide quietly in the body, a lack of adequate bile or impeded bile flow can make it hard for the body to break down fats which is important for individuals who are deficient in fat soluble vitamins like vitamin K2. As mentioned previously, a deficiency of vitamin K2 can lead to soft tissue calcification which might produce a wide variety of serious symptoms in the body.
Finally, a large number of patients have had their gallbladder removed. Without a gallbladder working to store bile, the liver must continuously produce large quantities of bile. It takes a lot of energy for the body to produce bile, which is why bile is typically re-circulated and recycled by the body. Bile that’s absorbed into the blood plays an important role in managing bilirubin and cholesterol levels in the body. But bile also plays a role in the absorption of fat soluble vitamins. A number of so-called “incurable” diseases today result from the use of bile sequestrant pharmaceuticals that doctors prescribe to their patients and the resulting fat soluble vitamin deficiencies that happen because there isn’t enough bile in the body to digest fats into bioavailable vitamins.
Bile is secreted from the liver and the gallbladder (in patients who still have a gallbladder) into the small intestine, but the duct through which bile is secreted from the liver and the gallbladder into the small intestine is shared via a common outlet with the pancreas. The Ampulla of Vater is the name of this common outlet for bile and pancreatic enzymes. This outlet can get plugged by a gallstone, which can easily be remedied using the Hulda Clark gallbladder cleanse. The outlet can also develop a stroma or other types of obstacles to bile flow. Bile flow and pancreatic enzyme flow can be partially or totally obstructed by gallstones causing a backflow of enzymes backward into the liver and the pancreas which can lead to serious problems. It’s worth noting however, that a cancerous tumor at the Ampulla of Vater is extremely rare due to the frequent passage of pancreatic enzymes through this area of the body.
Nonetheless, it’s easy to imagine how something as small and manageable as a gallstone can cause serious illness. If the reader also considers the fact that the liver and gallbladder are areas of the body that are easy to colonize by pathogens and that are nearly impossible to treat using antibiotics, and the fact that the liver is situated just below the diaphragm and the lungs and that it is relatively closely connected to the lungs, and the role of the liver in lung health becomes easier to recognize. Reactive oxygen species medicines can and should be used as an alternative to antibiotics in patients who suspect that they have a colony of pathogens living in the liver or the gallbladder.
Chronic Pulmonary Obstructive Disorder (COPD) and Asthma
Patients with COPD have been shown to be significantly more likely to develop or already have irritable bowel syndrome or irritable bowel disease than people without COPD. The instance of IBS or IBD in people with COPD is statistically higher than it is in people without COPD. The same is true for people who suffer from asthma.Both COPD and IBS/IBD are diseases that involve chronic inflammation of the mucosal tissues. In COPD, the mucosal tissues of the lungs are chronically inflamed, while with IBS or IBD, the mucosal tissues of the intestinal tract are chronically inflamed. There are many lymphatic vessels and tissues present in mucosal tissues, which further supports the connection noted above in regard to the direct communication between the lungs and the gastrointestinal system. One discussion in particular about the connection between these two illnesses calls COPD a kind of “pulmonary manifestation of IBD”, suggesting that the two diseases are, in some ways, the same disease manifesting in different areas of the body. By treating one, the other is likely to disappear, too.
COVID-19 and Other Coronavirus Infections
One of the primary ways that the COVID-19 virus damages the body is by binding with ACE2 (angiotensin-converting enzyme-2) receptors. These receptors are found in the highest numbers in the lungs and gastrointestinal system, and therefore these areas are where the virus tends to wreak the most havoc. When the virus binds with these receptors, the ACE2 protein isn’t able to bind with the receptors anymore, meaning that it can’t do its job sending signals to regulate blood pressure, promote wound healing, and reduce inflammation in the body. Since the ACE2 protein is directly involved with inflammation regulation, when the COVID-19 virus binds with the ACE2 receptors, this leads to increased inflammation in the whole body, starting with areas where there are the highest number of ACE2 receptors (in the lungs and gastrointestinal system). The cytokine storm is a good example of how the COVID-19 virus can cause damaging inflammation in the entire body, and particularly in the lungs and gut.One study observed that the incidence of hospital admission due to a COVID-19 infection was significantly higher in people who also suffered from some kind of gastrointestinal disturbance prior to infection. Additionally, patients who developed a COVID-19 infection also exhibited gastrointestinal symptoms as a result of the infection were also more likely to be hospitalized (note also that an infection with COVID-19 can lead to gastrointestinal problems where they weren’t present before).
Pneumonia
Pneumonia can be caused by a virus or as a result of other types of pathogens like bacteria or even fungi. In either case, the microbiota of the gut and lungs and the communication between the two can make a difference between developing and not developing pneumonia in the first place. Recovery from pneumonia also typically involves healthy microbiota changes in both the lungs and the gut.In one study on 235 total people, the administration of probiotics to patients in the test group who had developed ventilator-associated pneumonia (VAP) resulted in a significantly lower number of microbiologically confirmed VAP cases. Only 36% of the people in the test group tested positive for VAP while 50% of the people in the control group (who had not been given probiotics) tested positive. Previous studies have also had similar results when administering probiotics to patients with VAP. In this specific study, the patients received one 500mg capsule three times daily containing live strains of Bacillus subtilis and Enterococcus faecalis (this particular probiotic was known as Medilac-S). It was administered via a nasogastric feeding tube for a total of 14 days in addition to the other conventional treatments that were administered to the control group.
Colds and Flu
The common cold and seasonal influenza are extremely common and both tend to involve respiratory symptoms of some kind. Seasonal influenza also sometimes involves gastrointestinal discomfort, such as vomiting or diarrhea, in addition to respiratory complaints. There have been some limited studies into the correlation between taking probiotic supplements and the incidence of colds and flu during cold and flu season. Most of these studies have indicated that the incidence of the common cold or influenza tended to be lower among groups taking probiotic supplements, with one study in particular indicating that people taking a probiotic supplement did indeed fare better than those taking a placebo.Due to the connection between the gut and the lungs and respiratory system, it stands to reason that taking care of your gut health (by taking probiotics, eating a particularly healthy diet, avoiding antibiotics or other medications that can destroy helpful gut bacteria, etc) would be particularly valuable for your entire body’s health, but specifically for the health of your lungs and respiratory system and for preventing infection.
Asthma, Irritable Bowel Syndrome, and Neurodermatitis: What These Diseases Have in Common
In Traditional Chinese Medicine, the lungs and the gut are intimately connected. And indeed, this connection has been proven scientifically and is referred to in terms of the Gut-Lymph-Lung Axis. The health of the skin is also closely related to the health of the gut and lungs. As an example, the three diseases mentioned in this heading, asthma, irritable bowel syndrome, and neurodermatitis, are considered to be different manifestations of the same problem. In one case, the problem shows up in the lungs (asthma), in another situation it shows up in the intestines (IBS), and in yet another case it shows up on the skin (neurodermatitis).These three diseases are closely connected enough that they often occur simultaneously or one after another. If a person has asthma and then they develop IBS, they will have to first heal the IBS, then progress “backwards”, healing the asthma, before they’ll finally be healed (this is also known as “reverse cycling” and happens in a lot of different healing situations). Even scientific literature has acknowledged this connection, noting that asthma sufferers are significantly more likely to develop IBS than people without asthma (up to 20% more likely according to one study), and also that people with IBS are more likely to have or develop asthma than the average person. Other gastrointestinal conditions like gastroesophageal reflux disease (GERD) and eosinophilic esophagitis are also correlated with asthma.
One notable characteristic that asthma, IBS, and neurodermatitis share is their relationship to peptidoglycans. IBS and neurodermatitis (a skin disease that is remarkably similar to psoriasis) both likely involve leaky gut syndrome, a problem where the lining of the intestines becomes more permeable and allows toxins to seep back into the blood from the intestinal tract. Specifically, partly digested pathogens, known as peptidoglycans, are the primary culprit when it comes to inflammation in the digestive tract and on the skin. Interestingly, one animal study observed a connection between the development and severity of asthma symptoms and the presence of Peptidoglycan Recognition Protein 1 (PGRP-1). These proteins are able to bind to peptidoglycans and thereby kill harmful bacteria, and are also able to decompose stray peptidoglycans in the system.
The relationship between neurodermatitis and psoriasis should be noted. Approximately 80% of psoriasis patients are cured by the use of ox bile supplements. And a much higher percentage of patients (approaching 100%) are able to cure psoriasis permanently by taking ox bile with the herb Fumaria officinalis along with some sunlight and seawater treatments in a beachy location (a much more humane treatment regimen than what doctors typically prescribe). Patients with asthma, IBS, or neurodermatitis might want to consider working with scientifically proven cures for psoriasis because these various diseases are so closely related.
The Reproductive Organs - Lung Connection
Lugol’s iodine is a famous cure for asthma that has been covered up by Big Pharma for a century or more. Lugol’s iodine is a form of iodine that contains both molecular iodine and potassium iodide. Potassium iodide is, of course, a powerful expectorant when administered in super-high doses (300-600 mg 3 to four times daily), but Lugol’s iodine can be administered in lower doses on a daily basis to improve immunity overall and to balance reproductive hormones and thyroid hormones. The expectorant qualities of potassium iodide in high doses provides a thought-provoking look at why Lugol’s iodine in lower doses taken daily can be helpful in the treatment of asthma.
The AlivenHealthy Iodine Bible - Everything you need to know to get started taking iodine and more!
Asthma, Mucus, and Reproductive Organs
An expectorant is a medicinal agent that thins and loosens mucus. Guaifenesin is the most commonly used over-the-counter medication that conventional medicine doctors prescribe to patients with croup or other cough-related problems that have to do with sticky phlegm. Guaifenesin causes a number of unpleasant side effects (like digestive upsets, dizziness, headache, and nervousness) and it isn’t especially good for patients. N-Acetylcysteine (NAC), Acetylcysteine, and Cysteine in contrast, are an amino-acid treatment that have similar effects as Guaifenesin except they tend to enhance human health. NAC loosens and thins mucus throughout the body. Indeed, it has been used to promote fertility through its mucus thinning effects which promote sperm motility in the vagina and uterus.Thus, one connection between the reproductive organs happens via changes in the mucus not just in the respiratory system but also in the reproductive system. Though its true that NAC, Cysteine, and Acetylcysteine (which can be used interchangeably, though NAC is the most studied) potassium iodide also has the ability to thin mucus and cause it to “flow”. This might explain to some extent why Lugol’s iodine is such an important cancer cure, particularly in people with cancer of the reproductive organs, including breast cancer. Mucus serves an important function in the body as a liquid that traps toxins and removes them from the body. When mucus gets too sticky, the body struggles to detoxify itself.
Though many healers remind their patients to “drink a lot of water” following a treatment session because they know that water will decrease the concentration of toxins in the blood, many healers don’t realize that drinking water can also help thin mucus. But the type of drinking water is also important. Drinking water that contains electrolytes is better than drinking water that does not contain a lot of minerals. Mucus, after all is salty to taste in part because it contains electrolytes which are necessary for “flow”. Sea water supplements taken with drinking water can make a big difference in thinning mucus. Indeed, the use of hypertonic saline as a nebulizing agent can also be beneficial for some types of lung disease.
Lugol’s iodine and potassium iodide specifically rises to the top as the number one cure for asthma. A deficiency of iodine most commonly manifests in pre-adolescent boys, but by adulthood, asthma is most common in girls. This fact is what alerted doctors to investigate the role of reproductive hormone cycles and changes as the primary cause of the disease. Of course, the connection between mucus and potassium iodide is insightful, but the connection between iodine supplementation and reproductive hormone levels provide even greater insights into the connection between reproductive organs and the lungs.
Asthma is a disease that involves constriction of the airways in response to an allergen. Another way to look at this disease is to think of it as a hypersensitivity of the bronchial tubes to a trigger that causes the bronchioles to spasm (peptidoglycans perhaps?). This hypersensitivity is mediated to large extent not just by the presence or absence of specific reproductive hormones, but rather by changes in hormone levels. When reproductive hormone levels are in a state of change, patients become more susceptible to asthmatic attacks (at the end of a menstrual cycle or in the middle of the cycle at ovulation hormones change more quickly). In children, boys tend to experience more pronounced reproductive hormone changes. In adults, women experience monthly hormone level changes throughout their menstrual cycle. At the times of their cycle when hormones are changing the most rapidly, women are most likely to experience asthmatic attacks.
Iodine deficiency is another extremely common problem in the U.S. on account of the fact that bromine and fluorine are two halogen elements that compete with iodine in the body and that are ubiquitous in the food supply, water supply, and the environment, particularly in the United States. Both bromine and fluorine can cause hormonal abnormalities that can lead to asthma and symptoms that involve bronchial constriction. The presence of bromine and fluorine in the environment, water, and food supply as agents that work against the proper use of iodine and potassium iodide in the body should also alert readers to the fact that these substances can cause lung disease and problems associated with proper mucus production and proper detoxification of the body.
Though iodine deficiency is a recognized root-cause of asthma, there are a number of patients with chronic lung diseases that could benefit from potassium iodide supplementation (using either Lugol’s iodine or Iodoral–start with 6.25 mg and increase to 50 mg over the course of time) to reduce bronchial inflammation and constriction.
Click here to subscribe to the Living Database!
Resources: