MY MOM’S STORY
 As a medical writer who specializes in writing about controversial topics, I have a good sense of what’s hype and what’s not on the Internet. This ability to recognize the bullshit is really helpful to me in day-to-day life when everyone I love in the world is happy and mostly healthy. It’s easy to sift through all the crap to find information about things like toxins in shampoo, or how eating a gluten-free diet can totally change your life for the better. When there’s no time pinch and no emergency, I can wade through all the misinformation to find the good stuff. But recently, my mom started vomiting blood. She was bleeding profusely from her rectum. She passed out in a pool of blood. It happened very suddenly and there was little to no time to do research and try to figure out the best course of action for her. She was swept up into the hospital and transferred twice to bigger cities for procedures I’d never heard of before. I was on the road, driving or talking to doctors and I was grateful for every bit of information online that helped me and my family make decisions for my mom.
As a medical writer who specializes in writing about controversial topics, I have a good sense of what’s hype and what’s not on the Internet. This ability to recognize the bullshit is really helpful to me in day-to-day life when everyone I love in the world is happy and mostly healthy. It’s easy to sift through all the crap to find information about things like toxins in shampoo, or how eating a gluten-free diet can totally change your life for the better. When there’s no time pinch and no emergency, I can wade through all the misinformation to find the good stuff. But recently, my mom started vomiting blood. She was bleeding profusely from her rectum. She passed out in a pool of blood. It happened very suddenly and there was little to no time to do research and try to figure out the best course of action for her. She was swept up into the hospital and transferred twice to bigger cities for procedures I’d never heard of before. I was on the road, driving or talking to doctors and I was grateful for every bit of information online that helped me and my family make decisions for my mom.
My mom is not someone who watches what she eats. She thinks that alternative medicine is only a last resort and that it’s mostly fluff. Her lifestyle isn’t particularly healthy. But though she and I don’t agree on very many “medical” things, I still wanted to prevent her from being sold on a procedure that might kill her or leave her with a lower quality of life. She was stabilized initially at a tiny rural hospital before being transferred to a slightly better equipped hospital an hour away. There, they discovered that she was bleeding from an area of her small intestine just beyond the duodenum—an area that they couldn’t reach with the technologies available to them. So they transferred her yet again to a bigger hospital in a city four hours away. Again, I was on the road...driving, driving, driving.
At the new hospital, they used an endoscopy to try to find the bleeding. Because she’d vomited blood, the doctors felt like it was likely that the bleeding was coming from an area of the small intestine that was at least close to the stomach. This little piece of information—that she’d vomited blood--was important because it gave the doctors a clue about where the bleeding was coming from. And they had to find the bleeding to make it stop. It’s not possible for doctors to use a scope to go very far into the small intestine. Most of the digestive system is somewhat off-limits in terms of visual exploration. Even surgery is relatively limited in terms of what a doctor can find when a patient starts to bleed from the digestive tract. Opening up a patient’s belly to look at the OUTSIDE of the small intestine doesn’t offer many clues as to where bleeding is happening on the INSIDE of the small or large intestine. And when it comes to digestive bleeding, it’s all about finding the area that’s bleeding and closing it up. Sometimes bleeding ulcers do heal on their own, but we didn't know whether my mom's bleeding was an ulcer or some other problem. After the endoscopy, her doctors began thinking that it wasn't an ulcer at all, but rather an intestinal aneurysm that could cause her to hemorrhage to death at any moment.
Usually, blood in the small intestine doesn’t back up into the stomach unless there’s a major, MAJOR blockage in there. And it didn’t seem like this was the case since the blood had also been coming out of her rectum. If you ever have a family member who starts having intestinal hemorrhaging, keep this in mind as the doctors are trying to find the source of the problem. Did they vomit blood or did all of the bleeding come from the rectum? In the latter case, an endoscopy (a stomach probe) isn't probably as good of an ideas as a colonoscopy (an intestinal probe that only goes up into the large intestine and a small portion of the lower part of the small intestine). It seemed, for my mom, that the area in question was in the small intestine, near the stomach because my mom had vomited blood. Endoscopy and colonoscopy have some risks associated with them and they're unpleasant so advocate for your loved one. If the procedure seems superfluous, ask your doctor to explain his/her reasoning for using it. And if they can't sell you on the procedure, don't buy into it. After all, in the United States, health is a commodity...something that can be bought and sold like a used car... and you do have choices.
For the first 72 hours, my Mom's care was focused JUST on finding the area of the intestines that was bleeding. They gave her medication to reduce the stomach acid that she was producing (a drug that was like a stronger version of Prilosec--the doctors said the drug often stops ulcers from bleeding without further treatment) and my mom seemed to stop losing blood. Her vitals (blood pressure, pulse, oximeter, temperature, and respirations—these are usually calibrated on a machine that’s hooked up and on full display in the hospital room) were stable and this offered important clues about what was causing the bleeding. Good vitals meant that my mom was coping well with the blood loss. She probably didn’t have an infection. There was just bleeding---somewhere. Was it an ulcer or did she have a tumor? What there some other abnormality in her small intestine that was bleeding? The doctors were still thinking that it was an aneurysm.
At this point in the story, it's important that you know, dear Reader, that I believe that chemotherapy and radiation cause cancer. In fact, I don’t just believe it. I know it. As a medical writer and someone who regularly researches information on a variety of health-related topics, many of them controversial, I’ve learned that Big Pharma, Big Food, and Big Oil all rely heavily on cancer as a primary source of profits. Most normal people will walk--nay-- run from radiation and toxic chemicals when they don’t have cancer, but when they do have cancer, they sign up for loads of it to aimed at their bodies without hesitation. It doesn’t make sense because it’s illogical. Duh. I mean, when you really think about it, injecting toxic drugs into the body when it's already compromised and then inundating it with radiation does sound like a death sentence. But we want to believe that there’s a cure for cancer and chemo and radiation is all that the American public has been offered. The book I recommend to folks who’d like to connect all the dots on this topic and learn about non-chemo cancer cures (like the cancer “vaccine” RigVir in Latvia, or the BioMedical Center and Hope4Cancer clinics in Tijuana, Mexico, for example) is The Truth about Cancer by Ty Billington. This is a big and deeply disturbing topic that's beyond the scope of this article. We have also written a 3-book series that covers most of the major no-chemo, no radiation cancer cures that are currently accessible.
Onward...
ON NO MESH HERNIA SURGERY AND OTHER THINGS
I know that surgeons often insert gimmicky and “technologically sophisticated” things into patients’ bodies that can negatively impact their quality of life. This is important for people with abdominal/intestinal bleeding or for anyone undergoing surgery of any kind, really. You need to understand that the gimmicks are packaged as legitimate forms of treatment (and sometimes the “gimmicks” ARE legitimate forms of treatment depending on the situation). About three years ago, when our family was traveling down in Mexico, we went to the ruins at Uxmal where we encountered a man who kept holding his groin as he walked around looking at the pyramids and old stone structures. We tried to avoid him, but alas, he got into the van with us on our way back to Merida. But I’m glad he did. He and I talked for 2 hours and he told me that he had a hernia and he’d been trying to find a surgeon who would do the procedure without “The Mesh”. I hadn’t ever heard of The Mesh. I’d had a hernia as a young girl and the doctors had merely sewn up my abdomen with regular stitches. As a woman, I’d had a C-section too (which meant another hole in my abdominal wall, similar to a hernia incision, but much bigger) and the doctors had just sewn me up again. No Mesh. Twice I’ve had my abdomen opened up and sewn shut and after healing, I’ve gone about my super-active, over-the-top life without issues. But apparently, nowadays, doctors push The Mesh for hernias. It’s a metal fabric that can cause patients to experience autoimmune reactions like extreme joint paint and generalized inflammation in the body. Their sales pitch to patients goes something like this, “If you don’t get the mesh, your abdominal muscles might just pop open again at any time.” That’s enough to scare most patients into opting for The Mesh because they want a surgery that will be totally effective. But what the doctors say isn’t always true. Sometimes, the doctors simply make more money by selling patients The Mesh. They get a kickback from the pharmaceutical companies that push it (like, for example, a doctor who regularly offers The Mesh might get a free trip to a tropical location or something like that). I’ve done extreme weight training, marathoning, major and heavy construction projects in my home, and I’ve never ever thought about my hernia or C-section incisions as “weak” or ready to bust. Both were sewed up with regular stitches and healed normally and without issue. If you'd like to learn more about no mesh hernia surgery in the United States, click here.So this man at Uxmal had been to the U.S. in search of a surgeon, but he couldn’t find one, probably because he'd only searched at big hospitals in larger cities. My dad had a hernia this year and he was able to talk his doctor in North Platte, NE into doing the hernia procedure without The Mesh. North Platte is a small city though…barely a city at all. But I digress. My point is that there are lots of gimmicky medical “products” that doctors may want to insert into your body to make a procedure “less invasive” or “more effective”. don't buy into it unless you research it first and decide for yourself that it's the right thing for you, or unless you have no choice (as in a life-and-death emergency). This was the case with my mom. An endovascular surgeon in Lincoln, NE wanted to put a metal stent or coil into the vessels leading to what appeared to be an aneurysm in her duodenum. As far as I could tell, the metal stent didn't have the same horrible reputation for autoimmune reactions as The Mesh, but it did have a high rate of failure (around 30%). Later, after my mom was at home and recovering, when I went back and looked at the research, I found out that I was wrong. In fact, according to Grande and Stavropoulos (2006), “a substantial fraction of patients develop ‘postimplantation syndrome’ which consists of fever, leukocytosis, elevated C-reactive protein, and local abdominal tenderness in the absence of demonstrable infection” after an aneurysm coil is place in their bodies [1][2].
ON ANEURYSM COILING
My mom had been stable for two days before the aneurysm coiling procedure (also known as Endovascular Aneurysm Repair or EVAR) was proposed to me by the doctor. When the doctor came into the room he was selling the metal stent/aneurysm coil product as an option that was “less invasive” than traditional surgery, which, of course, is a big selling point. The stent would carefully be moved into position inside the vessels leading up to the aneurysm and then ejected into place at which time it would spring into the shape of a coil inside the vessel. The coil was made of materials that would cause blood to clot inside of it, cutting off the blood supply to the aneurysm. What kind of materials was it made of? A metal like platinum? Dacron and other materials? [2][3] I read that there were different materials that might make up the aneurysm coil. So I asked the doctor what kind of material my mom’s aneurysm coil would be made of, but he couldn’t tell me. In fact, he was put off by my asking. I don’t think anyone had ever asked him that question and he honestly didn’t know. The material used to make the aneurysm coil is pretty important though because there aren’t very many materials that can be put in place inside a human body long term without causing an autoimmune reaction of some kind. Aneurysm coiling can cause flu-like symptoms in recipients, for example [2].And there were other problems. The metal coil or stent has a 33% fail rate within ONE YEAR if you read the medical literature [1] An article I read at Medtronic admitted that “there is a small, but significant, risk of aneurysm rupture that is slightly higher than that of open-surgery aneurysm repair.” [4]
Complications related to aneurysm coiling in the aorta (it’s hard to find specific research about intestinal aneurysm coiling, but the procedures are similar) that were listed by this site included:
- Stent graft fracture
- Infection
- Rupture
- Blood leakage
- Inadvertent or inappropriate blood flow blockage
- Movement of the stent graft from its original placement site [4]
After the endovascular surgery, my mom would have to go in often (possibly several times a year) for CAT scans to monitor the coil [4]. The high failure rate and the required post-op care was unacceptable, in my opinion, since my parents both live 9 miles from a small, rural hospital that was barely able to cope with her heavy bleeding on this original instance of blood loss. Further, my mom’s vitals were great. So she was the perfect candidate for a traditional aneurysm surgery to just close up the vessels by opening up her abdomen and stitching off the area that was bleeding. Yes, this was a more invasive procedure with its own risks (general anesthesia, blood loss, death, etc.), but it was less likely to result in an autoimmune reaction or worse, a complete failure of the device to keep her from hemorrhaging to death.
ON FLUOROSCOPY AND CANCER RISK
But that’s not all. The stent would be placed in her body using fluoroscopy, a procedure that involves heavy and prolonged radiation exposure. Technically speaking, fluoroscopy is like an “X-ray movie” where a continuous beam of radiation is aimed at the body part being examined so that surgeons can see all the inner parts of the body without ever cutting into the skin. It sounds like a good deal until you think about the effects that prolonged exposure to radiation can have on the human body (burns, cancer, etc.). We’re talking about 2 hours (or longer) of continuous exposure to X-ray type radiation [5].I negotiated with the doctor to have him do a traditional surgery on my mom and sew up the area that was bleeding in a “traditional” way rather than diddling around with all the high-tech gimmicky stuff. Yes, the traditional surgery would be more invasive and thus Mom would have a longer recovery (by a few days, perhaps—but sans the chronic flu-like symptoms and danger of total stent failure that she might have with the fluoroscopy and coil arrangement), but I didn’t want her to be exposed to the radiation and the subsequent risk of cancer. I negotiated with the doctor to NOT do the stent. I was concerned about the risk of stroke posed by having a metal coil that might release blood clots into my mom’s system (he laughed at me, despite the research showing that this was a problem). He was resistant. I mean, “resistant” is an understatement. And he laughed/scoffed at me more than a few times (he was THAT kind of doctor). I never mentioned the cancer risk posed by radiation because most (practically all) doctors will deny that radiation and/or chemo cause cancer or that any radiation-oriented procedure aimed at healing would cause disease later. Read this report by the National Cancer Institute, and note that it mentions that staff and doctors don’t realize that fluoroscopy is also a hazard to their own health. I argued that the stent wasn’t a good choice and that traditional surgery was a better option. Eventually the doctor agreed. He left the room and then came back in with an ally to tell me that he wanted to do the endovascular surgery and the stent FIRST and then a traditional surgery afterwards because he was afraid that otherwise, using just the traditional surgery, the aneurysm might “pop” before he could sew it up. In other words, he wasn’t as familiar with doing a traditional surgery as he was an endovascular surgery that involved a stent. Apparently, according to the same report from the National Cancer Institute:
“Interventional fluoroscopy uses ionizing radiation to guide small instruments such as catheters through blood vessels or other pathways in the body. Interventional fluoroscopy represents a tremendous advantage over invasive surgical procedures, because it requires only a very small incision, substantially reduces the risk of infection and allows for shorter recovery time compared to surgical procedures. These interventions are used by a rapidly expanding number of health care providers in a wide range of medical specialties. However, many of these specialists have little training in radiation science or protection measures.” [5]
In other words, doctors who don’t have any experience or training in radiation-related work are being trained to use fluoroscopy. I’ve seen this kind of thing in other areas of medicine, like plastic surgery. Any doctor can make a switch to becoming a plastic surgeon even if their specialty is something like proctology or cardiology. They just hang out a shingle. And then, though their life’s work and education is on working with the heart, or the rectum, they go for a weekend training to do something like SmartLipo or what-have-you. It’s confusing to patients who naturally believe that their plastic surgeon is, in fact a plastic surgeon and not a general practitioner. Or, in this case, for patients who believe that their fluoroscopy doctor is someone who specializes in fluoroscopy and not just some doctor who did a weekend seminar on it.
In the end, with my mom, there was a compromise. I didn’t like it, but ultimately, the decisions were not mine to make, but my parent’s. This particular surgeon and his ally did a fluoroscopic exploratory surgery to find the exact location of the bleeding in my Mom’s intestines. His intent was to put the metal coil into the vessels that were feeding the intestinal aneurysm during the same procedure. The metal coil would reduce blood flow to the aneurysm which would make the next phase of the procedure less risky (since the aneurysm could “pop” and then my Mom could theoretically bleed out on the table). The plan was then for the doctor to go in and do a traditional surgery to sew the metal coils into place at either end of the vessels, thereby eliminating the high failure risk. We all (my brother, my husband, my dad, and my mom) agreed to this plan, but when the surgeon did the fluoroscopy, he couldn’t find an aneurysm. So he didn’t put the metal coils into my mom’s vessels (whew!). That was the good part. The bad part was that she was still exposed to all that radiation.
I think it’s important to put this story out there so that people can understand that medicine and surgery is still a creative process for doctors who are willing to entertain the possibilities of their craft. What the doctor offers you is not usually the ONLY answer to the problem. And it’s important to realize that “less invasive” or “minimally invasive” isn’t always better. Higher technology just simply isn’t always better. On the other hand, fluoroscopy is an amazing technology. It can save people’s lives. I acknowledge that. If a patient is bleeding and fluoroscopy is used as a last resort to find the source of the bleeding then, in this scenario, fluoroscopy plays the role of the good guy. Cancer comes on slowly and there are things you can do to prevent it and treat it without chemo or radiation (see the book The Truth about Cancer by Ty Bollington our our 3-book series for more info on this) if you have to be exposed to high-tech, radiation-rich-medicine like fluoroscopy. In cases of aneurysm in the aorta or in other large vessels or the brain, those metal coils can be life-saving. The technology, when properly applied is truly awe-inspiring. But it’s important to realize that some of these great technologies have a high failure rate or other consequences (like autoimmune reactions that can make life a form of hell) and that these future consequences would need to be addressed somehow after they save the patient’s life. The doctor didn’t tell us this. Most doctors won’t. The report from the National Cancer Institute says that doctors should. But I honestly even doubt that our doctor even knew about the consequences of fluoroscopy or the metal coils based on his reaction to me when I presented the information to him. And that’s not uncommon. Doctors buy into the gimmicks and the surgical products because they’ve been sold on them too. They learn how to use the gimmicks and then the pharmaceutical companies pat them on the back and give them kickbacks.
In the end, my mom didn’t have an intestinal aneurysm. She had a stroma, or a benign tumor with a bleeding ulcer on top of it. I had to leave the hospital on the other end of the state and go back home before the next set of doctors came in to offer her the next set of treatments and procedures. In the end, my mom and dad bought into a procedure that involved removal of the small intestine where the stroma was located. In other words, she was given two endoscopies, an endovascular surgery with fluoroscopy, AND she ended up having the traditional surgery to fix the problem in the end anyway. And I wondered: why couldn’t they have spared her the agony of 2 endoscopies, a fluoroscopy surgery, 3 days of not eating, and 5 days of sitting in the hospital inert and just removed that portion of the intestine in the first place once they’d determined that this was where the bleeding was coming from back on day 2 of the ordeal? It may seem like they were doing her a favor by trying “minimally invasive” options, but endoscopy (the stomach scope) is a risky procedure. It may be non-invasive, but a digestive “puncture” can kill a person. Fluoroscopy exposed my mom to radiation and a heightened cancer risk. Endovascular surgery is full of risks. And after over seven days in the hospital, she’ll have somewhere between $100,000 and $200,000 worth of medical bills to pay at the age of 64…right when she and my dad need their funds for retirement.
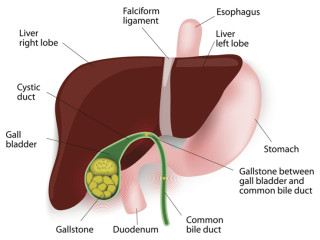
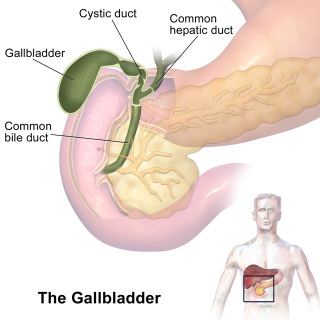
ON GALLBLADDER REMOVAL
And the doctor who did the surgery to remove the bleeding area of her small intestine went ahead and just removed her gallbladder too because “all it does is cause problems anyway”. I haven’t had the heart to tell my parents that gallbladder removal further elevates my mom’s cancer risk because excess bile salts are carcinogenic. Follow the link and read between the lines (that’s what I do for a living)…the ”controversial studies” about the link between gallbladder surgery and right colon cancer is worth considering. What’s the controversy? The fact that the AMA and Big Pharma don’t want you to know that gallbladder removal can lead to a heightened risk of cancer. How high is the risk? I don’t know. But you should keep this in mind and use your best judgment if your loved one is on the surgical table.I don’t see any good that could come from telling my mom about gallbladder removal and cancer (or chronic diarrhea, which is another fun side effect that happens to some people after gallbladder removal) since she didn’t have a choice about it, but I’m telling you so you can prevent your loved ones from these medical errors. If a surgeon does a procedure on you or your loved one’s abdomen tell them YOU DON’T WANT THE GALLBLADDER REMOVED UNLESS THERE’S SOMETHING SERIOUSLY WRONG WITH IT. And even if the gallbladder has some stones, there are ways to get rid of those stones without surgery. The gallbladder is there, in our bodies, because it serves a function (storing and then distributing bile from the liver). My mom’s vitals were so perfect even as she was bleeding out. And through her entire life, she’s never complained about digestive issues related to her gallbladder. It sickens me that this doctor removed AN ORGAN without my parents’ permission. My parents, of course, thought they got a good deal…a “free gallbladder surgery”, but I’m sure the doctor charged them for it. Update 2021: See this article on the gallbladder and the use of ox bile as a way to support your digestive system and entire body after gallbladder surgery and/or removal. If you find yourself in a situation where your loved one has an intestinal aneurysm or a bleeding ulcer or any other kind of bleeding from the intestines or the stomach, just remember, “less invasive” and “minimally invasive” isn’t always better. High-tech isn’t always better. But sometimes they are. If the patient has poor vital signs or if they don’t seem like they’d be able to tolerate an invasive surgery with general anesthesia, then “less invasive” might be better. These decisions require critical thinking and intuition. Think about the long term effects. Making this decision requires the love and compassion that only loved ones can give. Beware of gimmicky surgical products like The Mesh for hernias or aneurysm coiling and fluoroscopy. The coil has its place and it can save lives, but like many things, it’s overused. Could a mere surgical stitch do the job, or maybe even complete removal of an abnormal area, instead of high technology? Keep in mind that most of the tissues in the body will heal themselves if properly stitched. Ask your surgeon to be creative and don’t settle for sub-par procedures designed to make you or your loved one into a repeat customer.
Related Posts:
References:
[1] Grande, W. & Stavropoulos, W. S. (2006). Treatment of Complications Following Endovascular Repair of Aortic Aneurysms. Available online: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3036361/ [2] Hayoz, D. Do, D.D., Mahler, F., Triller, J., Spertini, F. (1997). Acute inflammatory reaction associated with endoluminal bypass grafts. Available online: https://www.ncbi.nlm.nih.gov/pubmed/9418198 [3] Johns Hopkins Medicine [n.d]. Endovascular Coiling for Brain Aneurysms. Available online: http://www.hopkinsmedicine.org/neurology_neurosurgery/centers_clinics/aneurysm/treatment/aneurysm_endovascular_coiling.html [4] Medtronic (2017). Benefits and Risks – Endovascular Stent Grafting. Available online: http://www.medtronic.com/us-en/patients/treatments-therapies/stent-graft-aaa/benefits-risks.html [5] National Cancer Institute (n.d.) Interventional Fluoroscopy: Reducing Radiation Risks for Patients and Staff. Available online: https://www.cancer.gov/about-cancer/causes-prevention/risk/radiation/interventional-fluoroscopy.pdf